Complaints are rolling in about the high-cost interface fees charged by EHR companies for federally mandated connections
It won’t surprise pathologists and clinical laboratory managers to learn that vendors of electronic health record (EHR) systems are milking physicians and other health-care providers with excessive fees above and beyond the EHR cost. Vendors are socking it to providers—including medical laboratories—in the pricing they charge to create the mandatory interfaces required for the EHRs to connect with outside networks.
These excessive fees were the subject of a story published by Modern Healthcare. It reported that healthcare providers contend that the interface fees are excessive because the software developed for federally mandated connections are common to all vendor customers. Therefore, the interfaces are used over and over again.
Interface Fees Criticized by Medical Groups
Michael Burkey, Director of Operations for Braddock Medical Group in Cumberland, Maryland, told Modern Healthcare that his six-physician, primary-care practice has “gotten killed” by interface fees. The group paid $5,000 each for interfaces to connect with the state’s public health registry and a patient portal, both of which are Stage 2 Meaningful-Use requirements for federal EHR incentives, “Across the board, everyone I’ve talked to, it’s the same problem,” he added. “Providers with the same brand EHR are going to pay the same prices I paid.”
But some physician groups consider certain informatics connections so essential that they don’t begrudge paying the interface fees. Eric Weidmann, M.D., the HIT champion at the South Austin Medical Clinic, in Austin Texas, told Modern Healthcare that the clinic’s EHR is connected to three medical laboratories, all of which involve complex HL7 interfaces. Noting the usefulness of these connections, he said, “For a few thousand dollars it’s well worth it having a more sophisticated, clean, timely system.”
One HIT Expert Calls the Added Fees an ‘Interface Scam’
Consider the number of interface connections required for EHRs to function, ranging from electronic prescribing and medical lab tests to other services noted Jason Mitchell, M.D.. He is the Director of the Center for Health Information Technology at the American Academy of Family Physicians. Mitchell suggested that “the interface racket is pretty significant. I asked a vendor last year, ‘Why are you charging our members $3,000 to $4,000 for interfaces and the ongoing cost of maintenance?’” He told Modern Healthcare, the answer was “because they can.”

Jason Mitchell, M.D., (pictured) faults federal regulators for not requiring EHR vendors to include the cost for mandatory EHR connections in their prices to qualify for the federal incentive program. (Photo copyright American EHR Partners)
Vendors Contend Interface Fees Only Cover Their Costs
To no one’s surprise, informatics vendors have a different take on the situation. Girish Kumar Navani is the CEO and co-founder of eClinicalWorks, an EHR developer based in Westborough, Massachusetts. He defended his firm’s interface fees, saying, “I have a team of at least 135 support people only supporting ancillary systems like labs, so it’s not inexpensive. I don’t think we run the interface end on a for-profit basis,” he added. “We just see that there are enough resources to keep it going.”
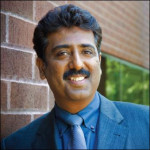
Girish Kumar Navani (pictured), CEO of eClinicalWorks, contends that the interface fees charged for connecting physician practices to laboratories and other healthcare services only covers his company’s costs. (Photo copyright CIO.com.)
Laboratories Often Get the Bill for LIS-to-Physician-EHR Interfaces
Pathologists and clinical lab managers won’t be happy to hear Navani’s philosophy about who should pay for the interface between a clinical lab and a physician’s office. Navani said that his company never charges doctors a fee, but rather asks medical laboratories and dictation companies to pick up the cost of interfaces with physician clients.
Navani does this “because they [labs and dictation companies] know they’ll make a lot of money from the physician practice down the line.” But this philosophy also puts clinical laboratories between a rock and a hard place: if they refuse to pay the interface fee, their physician clients are apt to take their business to a competing lab that will pay the interface fees.
Medical laboratories spend tens of thousands of dollars to interface their own laboratory information systems with EHRs. They do this despite the fact that there are no federal incentives to offset these costs. Paying for physician interfaces adds another financial burden to medical laboratories, which are already challenged to maintain quality amid cuts in reimbursement and increasing demand for lab testing services.
ONC’s Role in Creating This Problem
Since the cost of connecting one health information technology (HIT) system to another presents a major barrier to achieving Health and Human Services’ (HHS) goal of a national health information exchange, Mitchell faults federal regulators for creating this problem. “With all the criteria imposed on developers to qualify their systems for the federal EHR incentive payment program, “the cost of the EHR should have included all these interfaces,” he opined. “Hopefully, we’ll see some change coming, but I’m not holding my breath.”
Modern Healthcare pointed out that, in the latest round of rulemaking for EHR incentives, the HHS’ Office of the National Coordinator for Health Information Technology (ONC) stopped short of requiring vendors to provide all necessary interfaces to qualify for participation in the program. Previously, a proposed ONC rule would have forced vendors to reveal the full cost of products to potential customers.
In announcing the final rule in September 2012, the ONC called for price transparency as a guiding principle. However, the federal agency only required vendors to disclose the types of additional costs, but not the actual dollar amounts, noted Modern Healthcare.
ONC spokesman Peter Ashkenaz suggested that, when shopping for an EHR product, medical providers should ask vendor salespersons to provide details on all add-on fees they will be liable to pay. He also recommended that providers report those vendors who are not forthcoming about added costs.
The Modern Healthcare story pointed out that there are vast differences in pricing from vendor to vendor. While $5,000 appears to be the average fee charged for an interface, Amazing Charts, an EHR developer in North Kingstown, Rhode Island, charges labs $5,500 for the first connection to a physician practice. That is to cover the cost of building high-level HL7 interface software. After that, Amazing Charts only charges $500 for each additional physician connection.
Add-on Fees May Slow Expansion of EHRs and Vendor Profits
EHR vendors may be shortsighted in their interface pricing policies. Rick Blume, Managing Director of Excel Medical Ventures, a Boston-based venture capital firm, suggested that EHR vendors apparently don’t see the bigger picture and that, in the long run, interoperability is good for their business.
He told Modern Healthcare, that with EHRs, certain companies are “trying to salvage their backbone product” by increasing ancillary revenues from things like interface fees, “instead of stepping back and saying we’d be money ahead if we made this open architecture.”
Unfortunately for the nation’s clinical laboratories and pathology groups, they will probably continue to pay for the interfaces needed to connect their lab systems to the EHRs of their client physicians. That will continue to an expensive part of doing business as physicians acquire and implement EHR systems for their medical practices.
—By Patricia Kirk
Related Information:
How much is this going to cost me?
OIG allows hospital to give physicians access to free EHR interface




This issue looms like a dark cloud over our operating budget as the cost of connecting to our clients diverse EMR systems will reach more than $70,000 in 2019. With PAMA cuts taking 10% in 2018 and another 10% in 2019, adding EMR connections has added a sting to the bite. We were able to write our own in-house system to manage the HL7 messaging system, otherwise we would have had another vendor to pay for that piece. I’m encouraged that there is at least an awareness of the problem and hoping someone will put forth some real solutions to help labs like ours with these costs.
Steve Price, Chief Technology Officer
Interesting article that represents the general frustration and issues with interfaces with reference laboratories.
What is unsaid, however, is that interfaces are complex and an interface to one instance of an EMR system is not the same as an interface to another instance of the same EMR to the same reference laboratory. Current levels of standard terminology and varying interpretations (vendor implementations) of HL7 standards preclude a more efficient process.
As an informatician within a reference lab and a former EMR vendor, I have seen this situation replay itself time, and time again.
Significant improvement to LIS design, EMR design and interface tools are needed to bring costs down.