A part of this legislation, the grandfather clause on Technical Component (TC) anatomic pathology services was extended through June 1, 2012.
Last Friday, clinical laboratories got bad news about new cuts to the Medicare Part B medical laboratory test fee schedule. Congress voted on a temporary funding fix to keep Medicare physician fees at current levels for 10 more months and a reduction in lab test fees was one source of the money that Congress used to fund this bill.
Pathologists and clinical laboratory managers will be disappointed to learn that the Medicare Clinical Laboratory Fee Schedule (CLFS) was cut by 2% when Congress voted on Friday, February 17, to approve a deal to extend the payroll tax cut for nine months. President Obama could sign the bill into law today (Monday, February 20). The cuts to lab test fees are estimated to total $2.7 billion over 10 years.
Clinical Laboratory Industry Unprepared for Swift Legislative Action
The cuts caught the clinical laboratory industry off guard because of the speed with which Congress acted. “These specific cuts were proposed on Tuesday, February 14, and then included in the final bill by Thursday,” stated Alan Mertz, President of the American Clinical Laboratory Association (ACLA), in a telephone call with Dark Daily on Sunday, February 19. “The Senate voted 60-36 on Friday to approve the $145 billion payroll deal, just minutes after the House passed a similar bill 293-132,” explained Mertz.
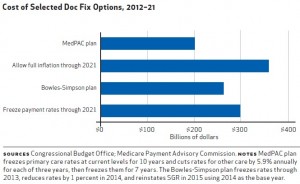
Last week, two little-known provisions that affect medical laboratories were included in the tax cut compromise legislation. These two provisions, along with other provisions in the bill were included in the bill’s language so that physicians treating Medicare patients did not face a 27.4% cut in the sustainable growth rate (SGR) formula and so that the payroll tax cut could be extended yet again. Physicians complained that the looming cuts to their Medicare payments of 27.4% would have triggered disruptions in their willingness to serve patients covered by the Medicare program.
The first provision that affects laboratories will reduce clinical laboratory payment rates by 2%, effective January 1, 2013. The estimated savings from this lab fee cut will be $2.7 billion over 10 years.
“The 2% cut exacerbates concessions that the clinical lab industry made in 2010 to ensure passage of the Affordable Care Act (ACA), observed Mertz. “At that time, labs agreed to a cut of 19% in the fee schedule.” (See Dark Daily, New Healthcare Law Cuts Clinical Laboratory Test Fee Schedule by 1.75% Through 2015, April 19, 2010.)
“Now comes this additional 2% cut in lab test fees, along with the potential for yet another 2% cut next year as part of congressional efforts to balance the federal budget,” explained Mertz. “Together, these cuts total 23% over 10 years.”
Robert Skinner of ML Strategies, government relations consultants in Washington, D.C., agreed that the latest 2 % cut surprised the clinical lab community. “Once word got out that the conferees were considering using the reduction, the Clinical Laboratory Coalition sent Chairman Max Baucus (D-Montana) of the Senate Finance Committee, a letter asking for their payment schedule to be spared, but to no avail,” Skinner wrote in the National Law Review.
Pathologists Get Extension on Technical Component Grandfather Clause
The second provision that affect labs allows independent labs that have an arrangement with eligible hospitals to bill Medicare directly for payment for the technical component (TC) of certain surgical pathology services, as opposed to billing the hospital, through June 30, 2012.
“This four-month extension provides time for the labs and hospitals to establish payment arrangements,” ACLA said in a written statement. “Expiration after a reasonable transition period addresses concerns that Medicare is paying twice for the same service, which causes beneficiaries to make an extra co-payment. Minimal CMS oversight of the policy has also made Medicare susceptible to making inappropriate payments. This provision would increase spending by less than $50 million from 2012 through 2022.”
After June 30, however, federal budget planners believe that ending this provision will help cut government spending. Mertz explained that one consequence of ending the TC grandfather clause is that those pathology labs currently providing TC services covered by the grandfather clause would then have to collect payment directly from hospitals after June 30, 2012. Events unfolded rapidly last week. “When ACLA learned of these cuts on Tuesday, the Clinical Laboratory Coalition had about 30 hours to lobby members of Congress,” stated Mertz. “The clinical laboratory fee cuts first appeared on Tuesday night and the ink was dry on Thursday.
Andrew Fish, Executive Director of AdvaMedDx, an advocacy organization in Washington, D.C., criticized the cuts because it will erode the quality of medical laboratory testing services and reduce access to testing by Medicare beneficiaries. “AdvaMedDx is strongly opposed to further cuts in the Medicare Clinical Laboratory Fee Schedule as has been put forward in the proposed ‘Doc Fix’ deal,” stated Fish. “The proposed cuts run counter to developing the next generation of lab tests that will allow treatments to be tailored to meet the needs of specific individuals, improving care and reducing costs.
Fish emphasized that the clinical laboratory industry has endured substantial reductions to the prices it is paid by the Medicare program. “The [Medicare Part B Medical] laboratory fee schedule is already facing five years of successive cuts under the Affordable Care Act continuing until 2015—resulting in a 9% cut, the largest cut among all Part B providers. We are gravely concerned that these additional cuts—estimated to provide savings of nearly $3 billion—will delay or deny patient access to life-saving and life-enhancing innovative diagnostic tests.”
More Congressional Threats Ahead for Medical Lab Test Reimbursement
It is not often that clinical laboratory managers leave their offices on a Friday night oblivious to events unfolding within the Capital building, only to arrive at work on the following Monday morning to learn the news that Congress has enacted a significant cut in Medicare Part B lab test fees. Yet this is not likely to be an isolated incident, given the ongoing federal budget crisis.
Pathologists and medical laboratory professionals will recall that a number of potential approaches to cutting reimbursement for laboratory testing have been identified by both houses of Congress. Still lurking out there is the proposal to institute the 20% patient co=pay requirement for laboratory tests provided to Medicare patients.
—By Joseph Burns
Related Information:
Clinical Labs Face Additional Fee Cuts in Final Payroll Tax Cut Deal
AdvaMedDx Statement on Proposed Medicare Clinical Laboratory Fee Schedule Cuts
Payroll Tax Deal Includes Cuts to Medicare Clinical Lab Fee Schedule Feb 17, 2012
New Healthcare Law Cuts Clinical Laboratory Test Fee Schedule by 1.75% Through 2015
Payroll Vote Gives Congress Nine-Month Breather on Tax Decisions
ACLA Urges Congress Not to Cut Medicare Payments for Clinical Laboratory Services




Here is yet more evidence that the Affordable Health Care Act will not be so affordable for healthcare service providers. This abomination deserves repeal at the earliest possible date.
Once again the Federal Government has chosen to ignore the contribution clinical laboratories make to diagnostic decision making and, yet again, reduce reimbursement for the testing provided. When one considers the level of cuts the laboratory industry has accepted over the past decade, it is both illogical and short-sighted on the part of the Federal Government to think that we can continue to provide the same level of service with continued decreases in revenue. Perhaps Congress should look at more personal issues such as their salaries and health care allowances to realize some of the significant savings that are needed. Congress could even look at reducing or eliminating some of the self-serving “pork barrel” aspects of their day to day work. I am sure that this would create far more revenue and far less negative impact on health care in our country.