Nearly 500 healthcare organizations nationwide to participate in payment bundling for 48 Conditions
Medicare’s largest bundled reimbursement project to date is now launching. Clinical laboratory executives and pathologists are watching for clues as to how these bundled payment arrangements will compensate the clinical laboratory testing done on behalf of patients whose care is covered by this latest Medicare initiative.
The Centers for Medicare & Medicaid Services (CMS) will commence implementation of Phase 1 of the Bundled Payments for Care Improvement Initiative. This will be a three-year project that will test the viability of a universal bundled payment system to improve coordination and quality of care and lower costs. It is also the largest bundled-payment pilot to date, with nearly 500 participants, according to a story published by Healthcare Finance News.
One major goal of this Medicare project is to begin moving providers from the current fee-for-payment model to a single, lump-sum payment model. This would be true for all Medicare Part A and Part B services provided during one episode of care.
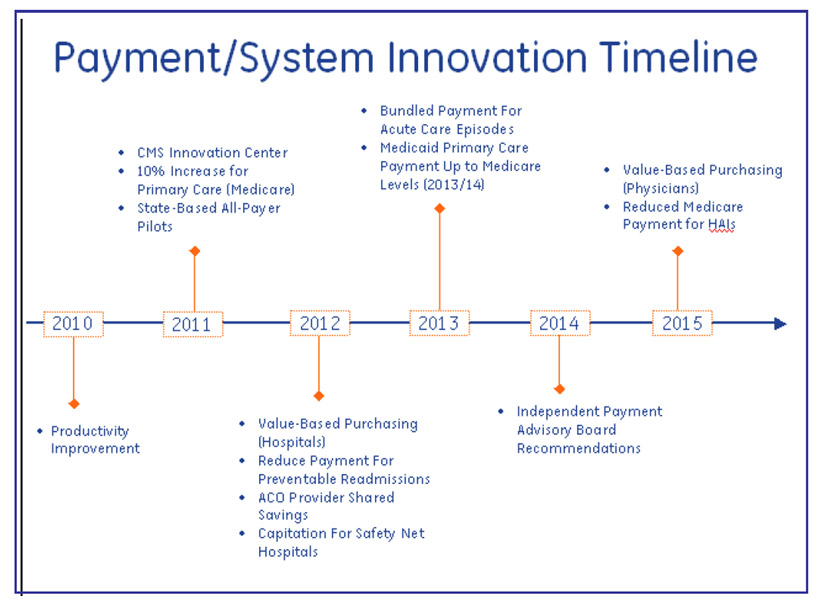
Medicare’s programs to reimburse acute care episodes via bundled payments are just one step forward in a planned implementation timetable for different forms of provider payment. At this time, there is not specific knowledge of how providers participating in these Medicare bundled payment programs will reimburse for the clinical laboratory tests provided to patients participating in these programs. (Graphic by Insure the Uninsured Project, itup.org.)
Some policy analysts fear that bundled payment arrangements would encourage hospitals to deny or skimp on services at the expense of patient care. However, as noted in a recent Modern Healthcare report, CMS will monitor results to detect inappropriate practices by providers. It will be watching for providers stinting on patient care or selecting patients in a way that maximizes financial gain.
Research Suggests Naysayer Fears Unfounded
Research has already demonstrated that bundled payments can align incentives for providers by encouraging them to work together across all specialties and settings. The expectation is that collaboration will reduce costs and improve quality because providers will develop care efficiencies. They can do this through quality improvement in clinical pathways and by improving the coordination of care.
Over the past few years, CMS has conducted smaller bundled-payment demonstration projects. However, these were only for a limited number of conditions, noted a DarkDaily.com report.
One example was a demonstration project for heart bypass surgery. It resulted in savings of $42.3 million, a savings of 10% less than projected costs, according to another DarkDaily.com e-briefing. Other benefits were improvements to the quality of care, significant declines in hospital mortality for the enrolled patients, and savings to the patients of approximately $7.9 million in co-insurance.
Large-scale Initiative Tests 48 Conditions in Four Patient Settings
Medicare’s newest bundled payment project will use four inpatient-care models. These will be differentiated by type of care provided and care setting. One goal is to test this payment model for 48 conditions, noted the Healthcare Finance News report.
• Model 1: “Retrospective Acute Care Hospital Stay Only,” includes an episode of care focused on acute care, inpatient hospitalization. Participating hospitals must agree to provide a standard discount to Medicare from the usual Part A hospital inpatient payments, and physicians are paid separately under the Medicare Physician Fee Schedule.
• Models 2 and 3: “Retrospective Acute Care Hospital Stay Plus Post-Acute Care” and “Retrospective Post-Acute Care Only, respectively,” involve a retrospective bundled payment arrangement where actual expenditures are reconciled against a target price for the episode of care.
• Model 4: “Acute Care Hospital Stay Only,” involves a prospective bundled-payment arrangement where the hospital receives a lump sum payment for an entire care episode and must pay other providers furnishing care out of this payment.
The CMS announcement marked the start of Phase 1 for Models 2, 3 and 4. It will run until July 2013. Phase 1 is a “no risk” period in which CMS will help participants prepare for financial and performance accountability for episodes of care, before entering the “risk-bearing” period of performance, explained the Healthcare Finance report. Phase 1 participants are expected to enter Phase 2 in July, at which time they will assume financial risk for episodes of care, pending contract finalization and completion of CMS’ program integrity reviews.
The Model 1 pilot will involve 32 hospitals and will test an expanded physician pay-for-performance program, beginning in April, noted Modern Healthcare. A second round of Model 1 testing is expected to start in early 2014.
Jeremy A. Lazarus, M.D., President of the American Medical Association (AMA), told Healthcare Finance News, “It is important that physicians in a variety of practice types have opportunities to participate in bundled-payment program pilots. We believe this initiative… presents an opportunity to improve the quality of care [for Medicare beneficiaries] and reduce costs,” he added, suggesting that CMS expand the program to outpatient medical settings.
No-Risk Period Allows Participants to Analyze Results Before Signing Up
Deirdre Baggot, R.N., MBA, Vice President at The Camden Group, a healthcare consultancy, and expert on bundled-payment applications, pointed out, in a HealthLeaders report, that the no-risk period provides an opportunity for participants to determine financial and readmission rates before agreeing to continue.
CMS, participants also will have the flexibility to select clinical conditions to bundle, develop partnerships across the continuum of care in their communities and determine how to redesign care delivery.
Readmission Policy Will Increase Provider Risk
Baggot noted, however, that CMS’ broader definition of readmission, to include all Diagnosis-related Group (DRG) codes, shifts more risk to providers. The bundled-payment program includes a standardized approach to defining 48 conditions, or converged episodes, that comprise 70% of hospital admissions, she explained.
The Centers for Medicare & Medicaid Innovation’s (CMMI) definition for related readmission holds the hospital of original admission responsible for readmission for 30 days following discharge. This is true regardless of why the patient is readmitted or whether or not the readmission is at a different facility. Baggot pointed out that the impact for episodes of care with a high rate of readmission, such as congestive heart failure, could exceed 20%.
Howard Gold, Senior Vice President of Managed Care at North Shore-Long Island Jewish Health System in Great Neck, New York, believes readmission risk can be lessened with staff training. He told Modern Healthcare, that his 11-hospital group, which is participating in the bundled-payment pilot, is focusing on nurse training and discharge planning to better manage care and costs. Gold believes his hospital group failed a previous bundled-payment experiment due to lack of this type of training.
How Clinical Laboratories Can Prepare for the Inevitable
Initially, only medical laboratories and pathologists affiliated with participating healthcare organizations will be affected by bundled-payment arrangements. But if all goes well, soon or later this payment model may be expanded to providers of outpatient services, including non-hospital-based laboratories.
These are reasons why other clinical laboratory administrators and pathologists would be smart to track the successes and failures associated with this new bundled-payment initiative. It will be important to understand why some providers were successful and others were not.
—Patricia Kirk
Related Information:
Bundled Payments for Care Improvement (BPCI) Initiative: General Information
Bundled payment initiative to lower costs, help coordinate care
Bundled Payments for Care Improvement (BPCI) Initiative: General Information
Bundled payment initiative to lower costs, help coordinate care
CMS Bundled Payment Changes Untenable?
Federal Officials Approve Applications for Bundled Payment Initiative
CMS Launches Payment Bundling Initiative To Improve Care, Cut Costs
CMS bundled payments pilot promotes better care coordination
Medicare Test-Drives a Single-Payment System in Four States
Medicare Test-Drives a Single-Payment System in Four States



