Hospital’s purchase of an “enterprise-wide solution” to be the EMR and related ancillary system software often leaves the hospital lab without the full LIS functions found in best-of-breed LIS products
DATELINE—PITTSBURGH, PENNSYLVANIA, Part II: Adoption of electronic medical record (EMR) systems by hospitals and health systems throughout this country may now be the single most disruptive factor in how hospital labs configure their laboratory information systems (LIS) specifically in support of their parent institutions’ informatics requirements.
This issue surfaced repeatedly during presentations made here on Friday, June 8, at the Strategic Summit organized by the Association for Pathology Informatics (API). In simplest terms, a growing number of hospital and health system administrators want to purchase and deploy a single “enterprise-wide solution” (EWS) for their EMR and total informatics needs.
Since the largest number of large medical laboratory organizations in the United States are based in hospitals or health systems, this is a significant issue for most clinical lab managers and pathologists. In Part 1 of Dark Daily’s reporting from the Strategic Summit, the trend of hospitals adopting EMRs was recognized as one of three primary developments in the field of clinical laboratory informatics. (See “All-Stars in Pathology Informatics and Clinical Laboratory Information Systems Gather in Pittsburgh to Assess Market Changes,” June 11, 2012.)
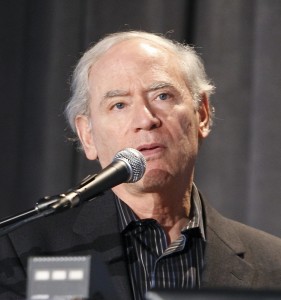
During his presentation at the Strategy Summit produced by the Association for Pathology Informatics last Friday in Pittsburgh, pathologist Bruce Friedman, M.D., called attention to the growing complexity of clinical pathology laboratory informatics. Friedman also discussed how the adoption of electronic medical record (EMR) systems by hospitals and health systems often takes place without a full recognition by hospital administration of the potential difficulties in creating an effective working interface between their institution’s choice of an EMR and the existing LIS. (File photo by DarkDaily.com)
What makes this market development both challenging and disruptive, however, is that some enterprise-wide solutions for a hospital do not have a robust LIS that supports the full functions needed by the state-of-the-art hospital laboratory. In such situations, the laboratory must supplement the LIS of the hospital’s enterprise-wide solution with a mix of software products and middleware from multiple vendors in order to serve not just the hospital inpatient testing needs, but also the requirements of blood banking, lab outreach services, and molecular/genetic testing, to name a few.
Threats to How Hospital Laboratories Currently Use an LIS
It was Bruce Friedman, M.D., Emeritus Professor of Pathology at the University of Michigan Medical School, who opened the day’s session and laid out the major issues that threaten to undermine the control clinical laboratories have over their information technology and laboratory information systems. “Most hospital administrators in the C-Suite lack an accurate understanding of the complexity that marks laboratory informatics,” he declared.
“I’d like to introduce a new term today,” said Friedman. “It is ‘T-LISF’ and stands for ‘total lab information system functionality. This describes the totality of all software-driven systems running in a lab.
“T-LISF is comprised of a classic, full-function LIS, along with middleware, outreach support, and the firmware that is integral to all automated lab testing lines and lab analyzers,” he explained. “Without T-LISF, all clinical labs and histopathology labs would cease working and most lab test reports flowing to physicians would stop.
“Hospital administrators discount the complexity to the T-LISF that supports every clinical lab and histopathology lab of size operating today in the United States,” observed Friedman. “They also fail to recognize that, because of the heterogeneity of T-LISF and the variety of information systems that are found in a complex laboratory facility, integration of all of these systems is difficult.
“It is the goal of a well-run lab to optimize the performance of its T-LISF to ensure patient safety and quality test results in a cost-effective operation,” he continued. “What threatens clinical labs is the desire of hospital CEOs to adopt a single enterprise-wide solution. This often means an electronic medical record (EMR) system which is fully integrated with the software that handles data from ancillary clinical services, including the medical laboratory, radiology, and pharmacy, to name three.
“When the hospital C-suite buys an enterprise-wide solution (EWS), they carefully analyze the financial implications of acquisition and implementation and they also want to reduce risk,” said Friedman. “However, the decision to purchase the EWS is often done without full consideration of the impact that the EMR system and its associated software modules may have on the operational and clinical efficacy of the hospital’s laboratory.
“In such instances, the hospital laboratory finds itself struggling to fully integrate its LIS to the enterprise EMR,” he noted. “If the EMR vendor has an LIS, that can further complicate things for the hospital lab if that LIS product lacks the full functionality of the several best-of-breed LIS products that are used by mid-sized and larger laboratories.”
Friedman’s recommendation to the participants was for hospital labs to work with hospital administrators to perform a gap analysis of institution and lab needs versus the capabilities of the proposed enterprise-wide solution (such as EMR and associated LIS product). “Along with the gap analysis, the lab team should be prepared to meet with the hospital administrators and present the total cost of a fully functional T-LISF. The discussion should include the consequences for patient care and clinician unrest if the proposed EWS project fails to meet the necessary objectives.”
In the next presentation at API’s Strategic Summit, Dennis Winsten of Dennis Winsten & Associates, Inc., tackled the same issue identified by Friedman. “If a hospital wants to purchase an enterprise-wide solution that is anchored by an EMR, how do the pathologists and lab administrators determine if enterprise-wide or best-of-breed LIS is best for their particular laboratory?” he asked.
Winsten has a unique perspective on this problem. During the past 24 months, he worked with several hospital clients to help them evaluate the relative merits and disadvantages of adopting an EWS that has a limited, but evolving LIS, versus acquiring or keeping a best-of-breed LIS.
“In each case, my client hospital had installed the EMR product sold by Epic Systems Corporation and had been offered a free site license for Beaker, the LIS developed by Epic,” noted Winsten. “Thus, the medical laboratories of these hospitals needed to provide the hospital CEO, CIO, and CFO with an objective and detailed assessment of what the institution would gain and lose by adopting the Beaker LIS rather than staying with the existing LIS.”
“Not all hospital laboratories will find Beaker—as it is functions today, suitable for all their needs,” observed Winsten. “The vendor acknowledges that Beaker is a work in progress.
Currently, this LIS is not as function and feature ‘rich’ as existing and mature LIS products. However, Beaker is evolving over time, according to established product release schedules. Thus, each hospital laboratory needs to understand what’s available now in the Epic ‘Beaker’ LIS, what is coming and when, and how the functionality and timetable will affect laboratory operations, quality, productivity, patient safety, service levels and outreach revenues.
Winsten continued, stating, “Several strategies for proceeding could include:
• ‘Wait and See How Beaker Evolves’;
• ‘Hybrid Combinations of Beaker and Best-of-Breed Components’; or,
• ‘Best-of-Breed Not Beaker’.”
The irony of this Strategic Summit is that Epic had no representatives—either as speakers or as attendees—in attendance. API organizers had invited Epic executives to speak at the program. In fact, this program was strongly support by four of the best-of-breed LIS vendors, who were: Cerner Corporation, McKesson Corporation, SCC Soft Computer, and Sunquest Information Systems.
Many of you emailed us after reading our Part I e-briefing about the disruptive forces now reshaping clinical laboratory and pathology informatics. In general, reader comments confirm that, as hospitals and health systems purchase electronic medical record (EMR) systems, the clinical laboratories of these institutions find it necessary to address a number of very serious operational and clinical issues. These reader comments confirm the observations by Bruce Friedman, M.D., that were presented above.
Your Dark Daily Editor,
Robert L. Michel
e-mail: rmichel@darkreport.com with your comments.
Related Information:
API Strategic Summit: The Future of Pathology Informatics and the LIS
Epic Challenge: What the Emergence of an EMR Giant Means For the Future of Healthcare Innovation



