Seeking ways to improve efficiency and cut costs, labs aim to use less formalin
One seldom-reported development in anatomic pathology is the new priority histology laboratories are giving to employee safety. Labs have long recognized that exposure to the dangerous chemicals used in processing tissue creates risk for histotechnologists.
Today, a rising number of medical laboratories in the United States and other countries are seeking to reduce those risks. Routine chemicals still used today in histology include formalin, toluene, and xylene.
National Cancer Institute Report Lists Formaldehyde as a Carcinogen
In August, a scientific body confirmed the risk of using formaldehyde in the workplace. The National Research Council of the National Academy of Sciences issued a report confirming findings in the 2011 National Toxicology Program (NTP) that listed formaldehyde as a carcinogen.
The report was titled: “Review of the Formaldehyde Assessment in the National Toxicology Program 12th Report on Carcinogens (2014).” This development is noteworthy for pathologists and histotechnologists and was covered in detail in a story published by the Chemical Regulation Reporter.
More specifically, on the National Cancer Institute website, laboratory technicians are among workers listed at greater risk of exposure to formaldehyde. Human studies provide sufficient evidence to conclude that exposure to formaldehyde can cause nasal and sinus cavity tumors as well as myeloid leukemia, according to the National Health Research Council. Some industry groups contest these conclusions.
Evidence Accumulating about Danger of Working with Toxic Chemicals
The accumulation of evidence about the danger of working with the toxic chemicals required for many methods of processing tissue motivates pathologists and clinical laboratory directors to make employee safety a high priority. At the same time, more companies are designing their histopathology systems and products to eliminate or use lesser quantities of such dangerous chemicals.
Take the example of formalin, which is a mixture of water and formaldehyde. Typically formalin must be present in the operating theater so that a surgeon, after collecting a patient specimen, can place it into a container with formalin to preserve that specimen during transport to the histology laboratory. Similarly, most pathology labs archive tissue specimens by storing them in buckets of formalin. These buckets are commonly sealed and stacked on shelves until the patient case is closed. These containers are then disposed of based on the facility’s disposal procedure.
An problem inherent in this approach is that buckets stacked in this way are susceptible to spillage and thus could compromise patient specimens. Formalin is inherently risky because—if spilled—formaldehyde gas is released, which is both toxic and flammable. Furthermore, formalin spills in operating theaters not only put the surgical team at risk of exposure, but require the exposed area to be sealed during cleaning. All of these events are disruptive to good clinical care and compromise the safety of hospital and laboratory personnel.
Vacuum-sealing Pathology Specimens in Spill-proof Bags
One alternative to storing specimens in buckets with formalin is to vacuum-seal specimens, with formalin, in bags so that they are virtually spill proof. Studies show that the use of this system requires less formalin, saving both material and disposal costs. More important, however, is that both the quality management of the patient specimen and worker safety for handling the specimens are greatly improved.
One company offering this technology is Milestone Medical, of Bergamo, Italy, and Kalamazoo, Michigan. It offers a patented vacuum specimen management system marketed worldwide. Surgical centers and pathology labs have their choice of either a system that vacuum seals specimens fresh or a system that vacuum-seals specimens with the option to add fixative into the bag at user specified volumes.
Reducing or Eliminating Formalin Reduces Histotech Exposure
“After seeing this system demonstrated, most pathologists and histotechs recognize the three primary benefits that an effective vacuum-sealing system can deliver,” noted David Sanford, General Manager of Milestone Medical Technologies Inc. in Kalamazoo, Michigan. “First, it gives them the ability to preserve, transport, and store tissue specimens with no formalin or much-reduced amounts of chemical preservatives. That improves worker safety in operating rooms and histology laboratories.”
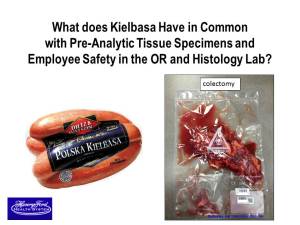
To drive home the point that vacuum-sealing of anatomic pathology tissue specimens is an idea whose time has come, pathologist Richard J. Zarbo,M.D., D.M.D., uses this graphic of a package of Kielbasa sausage and a colectomy tissue specimen. Both are in vacuum-sealed bags. Zarbo, who is the Chair of Pathology and Laboratory Medicine at Henry Ford Health System in Detroit, Michigan, then tells his audience that this proven technology allows pathology tissue specimens to be preserved with little or no formalin, improving safety for workers in operating theaters and histology laboratories. Vacuum-sealing of tissue has been routine for several years at multiple sites within the Henry Ford Health System. Zarbo presented this image during a recent Executive War College on Laboratory and Pathology Management (Photo copyright Richard J. Zarbo, M.D., D.M.D.)
“A second benefit is that it reduces the potential for formalin spills that can compromise specimens, and cut the expense associated with cleaning up such spills,” he continued. “The third benefit is that storage and eventual disposal costs of specimens in bags are greatly reduced.”
Some innovative pathology labs are adopting technology to vacuum-seal specimens in a variety of settings. “There is one large health system on the East Coast that is integrating our specimen vacuum-sealing technology in its core labs and multiple outreach-collection sites,” noted Sanford. “Some of the vacuum sealing equipment will be in labs and some will be in outpatient surgery settings. Primary use of these systems will be for specimen transport and for archiving after the specimens reach the histology laboratory.”
Reduced Formalin Use and Exposure at Henry Ford Health System
Another academic center—the Henry Ford Health System in Detroit—has used these vacuum-sealing systems for several years. “Our primary goal was employee safety,” stated Richard J. Zarbo, M.D., Senior Vice President and KD Ward Chair of Henry Ford Health System’s Pathology and Laboratory Medicine. “We have the added benefit of better specimen integrity and less cost because of our ability to reduce or even eliminate the amount of formalin we use.
“Another goal we are working on at the moment is to completely eliminate formalin from an operating room at our newest hospital, which is located 25 miles from the core pathology laboratory,” he added. “Also, there are three community hospitals in our health system that do not gross specimens, examine tissues, or process tissue locally. All tissues are sent to a centralized histology core laboratory. Vacuum-sealing systems are ideal in these settings.”
White Paper on the Use of Vacuum-Sealing Technology in Histology
Given the strong interest clinical labs have in cutting costs while improving safety, Dark Daily has published a white paper about the use of vacuum-sealing technology in histology laboratories and operating theaters. The white paper, Advances in Pathology Tissue Management Reduce Formalin Use, Improve Quality and Cut Costs, is available for immediate download.
As consumers, pathologists and histotechnologists buy perishable products at the grocery store that are vacuum-sealed to ensure freshness. This proven technology has improved food safety. Thus, the use of vacuum-sealing technology to preserve, transport, and archive pathology specimens is probably long overdue—and comes with the added benefit of reducing or eliminating the exposure to formalin that happens daily to most histotechnologists and pathologists.
—By Joseph Burns
Related Material:
Formaldehyde and Cancer Risk: National Cancer Institute
Formaldehyde Can Cause Cancers, Including Leukemia, National Academies Concludes



