Authors of the published study wrote that use of HD optical technology during colonoscopies gives patients a faster answer and may eliminate the need to refer biopsies to pathologists
High definition optical technology is reaching the point where gastroenterologists are able to identify pre-cancerous polyps with 96% accuracy during colonoscopies, according to a recent study conducted at the Mayo Clinic. Pathologists will want to pay close attention to the published findings of this study. That’s because GI biopsies represent a significant proportion of specimens referred to anatomic pathologists.
Researchers at Mayo Clinic worked with high-definition (HD) imaging systems, such as the Olympus Evis Exera II 180 and the Evis Exera III CV-190. The study was published in the June 24, 2014 issue of Gastrointestinal Endoscopy.
Experienced Physicians Identify Precancerous Polyps 97% of the Time
Using the Exera II 180, or its successor, the Exera III CV-190, gastroenterologists examined polyps in 522 patients. They were able to make a correct evaluation 96% to 97% of the time, reported a Mayo Clinic press release. The study was funded by Olympus America.
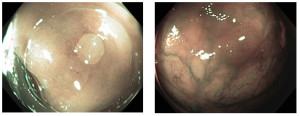
The benign (hyperplastic) polyp on the left appears very pale and bland on imaging, while the precancerous (adenoma) polyp on the right is darker with dilated blood vessels on the surface. (Photos and captions copyright the Mayo Clinic.)
With experienced physicians, an optical diagnosis, or “virtual biopsy,” was sufficient to distinguish between benign (hyperplastic) polyps and precancerous (adenoma) polyps, noted researchers at the Mayo Clinic’s Jacksonville, Florida, campus. Physicians participating in the study reported an extremely high adenoma detection rate using the scopes: 50% with the 180 model and 52% percent with the 190.
“A high adenoma detection rate is considered a good measure of a quality colonoscopy,” stated Michael Wallace, M.D., M.P.H., Professor of Medicine at Mayo Clinic Florida, Director of Mayo Clinic’s Digestive Diseases Research Program, and Editor-in-Chief at Gastrointestinal Endoscopy (GIE), in the press release.
Dr. Wallace was the study’s senior investigator. “Studies have shown that a rate of 33%—meaning that of 100 people who undergo a colonoscopy, adenomas are found in 33%—is excellent,” he explained. “Current national benchmarks recommend an adenoma detection rate of at least 20%. We found substantially more adenomas,” he added.
“The more adenoma polyps that are detected, the lower the risk is of getting colon cancer,” Dr. Wallace pointed out. “We discovered that gastroenterologists using high-definition optical scopes can provide excellent care and diagnoses of polyps without the added step of a pathological examination.”
Dr. Wallace continued, “Another advantage is that we can tell the patient immediately after the procedure what we found and when the next examination should be done, as opposed to waiting one to two days for a pathology result,” he said.

Michael Wallace, M.D., practices at both the Mayo Clinic Gastroenterology and Hepatology department and at the Cancer Center. “A colonoscopy is a fairly expensive procedure, and a large portion of the cost is the pathological analysis of polyps that are removed to check whether they are precancerous or benign—a check that determines when a patient needs another colonoscopy,” he stated in the press release. (Photo copyright the Mayo Clinic.)
Other Advances in Early Detection of Colon Cancer
Scientists have been working on various other methods of diagnosing colon cancer early as well. For example, proponents of virtual colonoscopy, or CT-Colonoscopy, a noninvasive procedure that uses CT-Scan of the lower body to detect precancerous polyps, got a shot in the arm by a study conducted at the Mayo Clinic in Scottsdale, Arizona. The study showed that this procedure effectively identifies both large and medium-sized precancerous polyps. Results of the study were published in a September 18, 2008, New England Journal of Medicine (NEJM) article.
And a University of Michigan study published in an August 7, 2014, Cancer Prevention Research article suggested that analysis of gut microbiome may be useful in diagnosing colon cancer, when combined with traditional risk factors, including body mass index, age, and race.
Additionally, use of automatic reminder technology built into electronic medical record (EHR) systems can improve timely cancer screenings. In a study by researchers at Group Health Research Institute in Seattle, Washington, use of the EHR to identify Group Health Cooperative patients due for colonoscopy stepped up interventions and doubled the rate of colorectal cancer screenings.
Cutting Out the Pathology Lab Could Cut Colonoscopy Cost Significantly
All of this advancement in colorectal cancer screenings might now be moot, as the Mayo Clinic researchers have concluded that the pathological polyp examination that is currently required by national practice guidelines might no longer be necessary, which could result in substantial cost savings for patients and the healthcare system, as well as quicker results and recommendations for patient follow-up.
It could also mean, however, that all other methods for early diagnosis of colon cancer could become unnecessary as well, which would significantly impact current cancer screening workloads at clinical pathology laboratories.
As a result of this study, the American Society for Gastrointestinal Endoscopy (ASGE) is reviewing current colonoscopy guidelines to decide whether pathological examination of polyps is necessary, Dr. Wallace stated. Should the ASGE alter its recommended protocol for colonoscopy, this could have a very disruptive impact on pathology groups, especially those performing a significant number of polyp analyses annually.
—Patricia Kirk
Related Information:
New Study Confirms Efficiency of Virtual Colonoscopy



