Multiple recent studies reveal a substantial number of patients continue to delay needed healthcare in the months since the onset of the SARS-CoV-2 outbreak
Based on an analysis of hospital emergency department (ED) usage, federal researchers concluded that patients continue to be cautious when visiting healthcare providers, including clinical laboratories, and that people are altering how they seek and utilize emergency care due to the COVID-19 pandemic. This not only reduces the number of typical test orders from the ER to the hospital lab, but also reduces the source of inpatient admissions.
The study, titled, “Impact of the COVID-19 Pandemic on Emergency Department Visits—United States, January 1, 2019–May 30, 2020,” found that ED visits declined 42% during the early stages of the COVID-19 pandemic. It was conducted by the federal Center for Disease Control and Prevention’s National Syndromic Surveillance Program (NSSP) and published in the CDC’s Morbidity and Mortality Weekly Report (MMWR).
Between March 29 and April 25 of this year, facilities the CDC examined recorded 1.2 million visits to EDs, compared to 2.1 million visits between March 31 and April 27 of last year. The steepest decrease in patient demographics was for individuals under the age of 14, women, and people living in the Northeast region.
The CDC’s data showed that 12% of ED visits were for children in pre-pandemic 2019, which dropped to 6% during the 2020 pandemic period. The CDC included ED visits from hospitals in 47 states (excluding Hawaii, South Dakota, and Wyoming) and captured information from approximately 73% of ED visits in the US.
Delaying Healthcare Visits Worsens Medical Conditions, Reduces Revenues
ED visits are an important referral source for inpatient admissions. Fewer patients in EDs means lost revenue for hospitals. However, one positive aspect of the waning number of ED visits is that it may be keeping patients with non-emergency situations away from emergency departments, thus reducing the overuse of costly ED visits. But healthcare professionals are concerned that individuals also may be avoiding or delaying care when needed, which could worsen medical situations and outcomes.
“We saw people, with COVID-19 and without, coming into the ED who were very ill,” Vik Reddy, MD, Chief Medical Officer at Wellstar Kennestone Hospital and Wellstar Windy Hill Hospital in the Atlanta area, told Modern Healthcare. He noted that some patients delayed care for critical non-COVID-19 illnesses. “The good news is that we’re seeing that trend reverse this time around. It was scary in March when we knew that people weren’t coming into the ED for heart attacks.”
The NSSP’s analysis concluded that the report’s findings were subject to at least four limitations:
- The number of hospitals reporting to NSSP changes over time as facilities are added or closed. For example, 3,173 hospitals reported data in April of 2019, while 3,467 reported data in April 2020.
- Diagnostic categories rely on the use of specific codes, which were missing in 20% of the ED visits reported.
- NSSP coverage is not uniform across or within all the participating states.
- The analysis is limited only to ED visits and does not take into account patients who did not go to an ED, but instead received treatment in other healthcare environments, such as urgent care clinics.
Additional Studies Show Patients Avoiding Hospital EDs, Delaying Care
Other sources also are reporting similar findings regarding consumer attitudes towards seeking medical care during the COVID-19 pandemic. A PricewaterhouseCoopers survey released in May found that about 45% of 2,500 consumers surveyed plan to forgo their annual physical in 2020, due to the pandemic, Modern Healthcare reported.
In addition, an Optum Consumer Pulse Survey released in May found that nearly 20% of 700 surveyed individuals stated they were likely to avoid hospital EDs even if they were showing signs of a heart attack or appendicitis. Another 40% stated they were likely to avoid the ED if they had a cut that required stitches.
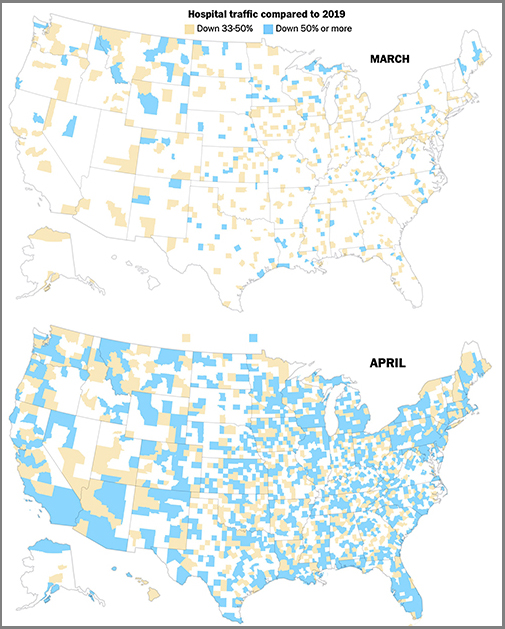
In “Americans Are Delaying Medical Care, and It’s Devastating Health-Care Providers,” The Washington Post analyzed hospital use during the pandemic based on smartphone tracking data. WaPo’s report found a significant drop in patients seeking in-person healthcare with many areas across the country reporting a 50% reduction in patients when compared to last year.
The article also states that almost 94 million people have delayed medical care due to the COVID-19 pandemic, and that 66 million of those individuals needed medical care unrelated to the virus but did not receive it.
These studies and others are showing a pattern. The COVID-19 pandemic has changed when and where patients access healthcare, and if the trend continues, it could have a long-term impact on clinical laboratories. Since fewer people are seeking medical care, fewer laboratory tests are being ordered and performed, which means less work and revenue for the nations’ hospital and independent clinical labs.
—JP Schlingman
Related Information:
Emergency Department Visits Continue to Lag
COVID-19 Caused Hospital ED Visits to Dive More than 40%
With Emergency Visits Down 42%, US Hospitals Reeling from COVID-19
How Patients Feel About Returning to Care
Americans are Delaying Medical Care, and It’s Devastating Healthcare Providers




