New technology could reduce or even eliminate the need for clinical pathology laboratories to utilize tissue biopsies in the diagnosis of certain cancers
“Cancer flashlight” is the nickname some have given to a system that uses novel spectroscopic techniques to detect pre-cancerous cells in the colon. Developed by bioengineers at Duke University, the device may offer an alternative to current biopsy methods for detecting cancer and pre-cancer by anatomic pathologists.
The new technology may be a way to detect abnormal, dysplastic cells in the epithelium of various tissues in a non-invasive way, wrote The Atlantic in a story it recently published. The Atlantic thinks this technology breakthrough may be significant because approximately 85% of all cancers begin within the layers of the epithelium in various parts of the body.
New Non-invasive Diagnostic Technology Uses Angled Light
Using angle-resolved low coherence interferometry (a/LCI), the new cancer “flashlight” is actually a component at the tip of an endoscope. It aims short bursts of light at tissue suspected of disease. Because the nuclei of pre-cancerous cells are misshapen and larger than normal cells, they scatter light in a unique way.
“When light is directed at these tissues, it scatters,” explained Adam Wax, Ph. D., Theodore Kennedy Associate Professor of Biomedical Engineering at Duke’s Pratt School of Engineering, who led the research team. “We can collect and analyze that scattered light looking for the tell-tale signs of dysplasia.”
Wax and his team presented the results of their pilot, ex vivo study online in the Journal of Biomedical Optics (JOBO).
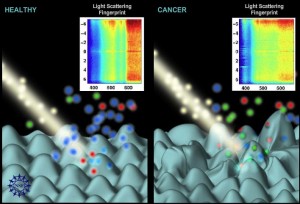
Researchers at Duke University used the “light scattering” fingerprints of a cell to identify cancerous or pre-cancerous cells. The technology is angle-resolved low-coherence interferometry (a/LCI). It is capable of measuring cellular apoptosis and can be useful in studying chemotherapeutic efficacy. (Image by Nicolle Rager Fuller, National Science Foundation.)
The Duke researchers first demonstrated accurate detection of precancerous cells in the esophagus. Later, they achieved similar results in detection of precancerous cells in the colon. One common problem with many current methods used to diagnose cancer is the need to collect a biopsy. The procedures used to collect tissue are invasive, can be dangerous, and, in some cases, even disfiguring and life-altering, the Atlantic story stated.
“The old-fashioned techniques we use haven’t changed in years. This could be a real game-changer in how we detect, characterize and even treat precancerous or cancerous lesions,” observed Christopher Mantyh, M.D., Chief of Colorectal Surgery at Duke University Medical Center and member of the research team.
The new “cancer flashlight” system is non-invasive and offers additional advantages. “The important thing for clinicians is being able to detect these changes in the nuclei in cells just below the surface, which might not be detected by just looking at the lining of the colon through an endoscope alone,” Wax explained.
The new approach could be especially useful for people with inflammatory bowel disease (IBD), Mantyh suggested. He explained that IBD patients tend to have a higher incidence of dysplasia in the colon. “For some gastrointestinal biopsies, the procedure itself has inherent risks, such as bleeding or perforation, so a non-invasive technique could greatly improve a patient’s quality of life.”
Innovative System Shows High Sensitivity, Specificity and Accuracy
In their experiments on colon tissue, the Duke team used the device on samples of colon removed from 27 patients suspected have having colon cancer. They then compared the results obtained to actual findings made by pathologists, the Atlantic writer wrote.
According to the JOBO article, the Duke scientists found a statistically significant correlation between increased average nuclear size, reduced nuclear density, and the presence of dysplasia at the basal layer of the epithelium, at a depth of 200 to 300 micrometres. In the experiments, the a/LCI technology was able to separate dysplastic from healthy tissues with a sensitivity of 92.9% (13/14), a specificity of 83.6% (56/67), and an overall accuracy of 85.2% (69/81), the article noted.
“This approach could be the future of diagnosing dysplasia of the colon,” speculated Mantyh. Wax believes the new system could also prove useful in detecting and diagnosing such cancers as those of the trachea, cervix, or bladder.
Another notable aspect of the angle-resolved low coherence interferometry (a/LCI) technology is that it represents a new methodology that has the potential to measurably reduce the number of tissue biopsies currently required to diagnose certain types of cancer. Of course, there would still be the need for anatomic pathologists and medical laboratory scientists to confirm positive findings and conduct additional molecular and genetic tests as needed to develop therapeutic options for additional patients.
—Pamela Scherer McLeod
Related Information:
The Best Ideas from Duke University: A Foldable iPad and a Cancer Flashlight
Detection of intestinal dysplasia using angle-resolved low coherence interferometry



