Pathologists and clinical laboratory managers should fundamentally change how cancer specimens are handled
Three physicians at Scripps Health are calling for pathologists to rethink how they collect and store cancer tissue samples in two significant ways. They say that pathologists need to: 1) move away from formalin-fixed, paraffin-embedded (FFPE) tissue blocks and toward frozen samples; and, 2) start collecting larger samples.
These doctors used the Journal of the American Medical Association as a platform to issue their call for a change in what has been a long-standing standard of practice in anatomic pathology. Given the progressive nature of these opinions, there will certainly be dissenting voices within the pathology profession who are likely to add their voices to this debate.
Genomics-based Treatment of Cancer Is Changing Clinical Practice
At an accelerating rate, genetics is making its way into strategies for treatment of cancer. “Genetic sequencing technology is altering the way cancer is diagnosed and treated,” stated Scripps Health in a recent news release. “But traditional specimen handling methods threaten to slow that progress.”
The source of the message was a column by three Scripps Clinic, published recently in the Journal of the American Medical Association (JAMA) “Standards for acquiring appropriate tissue samples …must evolve,” the authors declared.
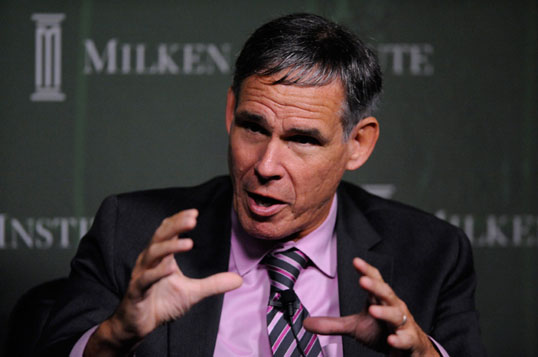
Pictured above is Eric J. Topol, M.D., professor of genomics in the Department of Molecular and Experimental Medicine at the California campus of The Scripps Research Institute. He and two colleagues are calling on pathologists to change the way they collect and store tissue samples from cancer patients. Additionally, he is on a mission to educate patients, patient advocates and consumers. He believes that, if patients understood the advantages, they could insist that pathologists and surgeons procure, process and store tumor samples in ways that are compatible with genetic sequencing of the DNA. (Photo by FasterCures.com.)
For decades, pathologists have used an FFPE approach. However, the authors pointed out that the chemical mixture of formaldehyde and water in traditional processing can degrade DNA. That makes it difficult or impossible to genetically sequence tumor tissue processed with formalin. Sequencing thus requires frozen tissue samples.
In the JAMA Viewpoint piece, the three Scripps physicians explained that discovering the crucial detail of critical driver mutations and biologic pathways allows for adjustment of a patient’s cancer regimen. But discovering those mutations and pathways can only happen with whole genome and exome sequencing of frozen tissue.
“As the new clinical applicability of genomics emerges at a fairly rapid rate, the field of pathology will arrive at the tipping point for a fundamental change in how cancer specimens are handled,” the authors wrote.
Increased Tissue Procurement and Higher Storage Costs
Currently, the trend is to perform less invasive procedures and to procure smaller samples, a story published at Medscape reported. However, tissue samples may need to be larger.
Research suggests that freshly frozen tumor tissue may increase the capability for more comprehensive genomic sequencing, the Medscape.com writer noted. That’s because single-tumor biopsies may give an insufficient view of the tumor genomics landscape, according to an earlier study published in The New England Journal of Medicine. This is significant because intratumor heterogeneity may foster tumor evolution and adaptation. Consequently, the study found, smaller samples could hinder personalized medicine strategies.
“Although it is vital to avoid performing excessive biopsies with serious adverse effects, the trade-off may be missing mutations that could alter the patient’s course of treatment,” the Scripps authors stated in the JAMA Viewpoint piece.
Pathologists Could See Patients Insist on Frozen Tissue Samples
“This is a really hot area, but the problem is the patients don’t know about this,” declared Scripps coauthor Eric J. Topol, M.D., a cardiologist and Chief Academic Officer at Scripps Health. Dr. Topol is also director of the Scripps Translational Science Institute (STSI) and heads Scripps’ genomic medicine research.
According to Topol, there is significant resistance among pathologists to adoption of frozen tumor sampling, the Medscape reporter wrote. There are at least two reasons. One is the higher costs associated with increased space, monitoring, and electricity for the storage of tissue specimens in freezers. Second, there may be problems with reimbursement.
Topol and his coauthors believe that more patients would likely agree to an increased cost of procurement if they understood that could mean better diagnosis and treatment.
College of American Pathologists’ President Speaks Out
“This type of change will require discussion about new operative standards,” stated Stanley Robboy, M.D., President of the College of American Pathologists (CAP), in the Scripps news release.
Topol emphasized that patients and healthcare advocates have a direct role to play in this transformation. “We need to call out patients, consumers, patient advocates to be knowledgeable about this, because they are the ones who can drive it,” he told Medscape.com.
Of course, anatomic pathologists can see for themselves how molecular and genetic methods are making inroads in diagnostics and clinical practice. It is therefore interesting that the three physicians at Scripps Health (and the editors at JAMA) considered it timely and relevant to publish an opinion piece that points out the need for the pathology profession to move more quickly to process tissue specimens without using formalin. Innovative medical laboratories will want to factor these developments into their strategic planning.
—Pamela Scherer McLeod
Related Information:
Rebooting Cancer Tissue Handling in the Sequencing Era: Toward Routine Use of Frozen Tumor Tissue
Scientists call for big change in cancer analysis
New Standards of Practice Needed in Cancer Tissue Sampling
JAMA column outlines need for frozen, larger specimens in DNA-sequencing era
Intratumor Heterogeneity and Branched Evolution Revealed by Multiregion Sequencing
What is THE DARK REPORT clinical laboratory intelligence charter membership services?




Of course it’s obvious that this is a self-serving call. With the way funding is being squeezed, traditional methods will be with us for a long time.
These people are misinformed.
First, “next gen” sequencing machines, e.g. the Ion Proton machine by Life Technologies, can use DNA extracted from FFPE tissues as starting material.
Secondly, the first information that both the patient and his doctors need is whether i) the biopsy contains the lesion, ii) if it is malignant or benign, and iii) what category of malignancy. “Next gen” sequencing provides an enormous amount of information. The report for a given specimen must be tailored to the type of tumour as determined histologically.
In my opinion, good histology will remain the first step in the diagnosis process.