Extraneous tissue cross-contamination found in all participating pathology laboratories Cross-tissue contamination, regardless of specimen volume or how frequently reagents were changed
Pathologists and histotechnologists have long known that traditional methods of processing tissue for diagnosis have the potential to cross-contaminate human biopsy specimens. This risk to patient safety and diagnostic accuracy was accepted over the decades because of the limitations of technology and inability to more precisely measure the performance of individual work processes in the histology laboratory.
In recent years, two things have begun to change this long-standing status quo in medical laboratories. These developments now make it possible to more accurately measure the performance of histology work processes. In turn, this allows an understanding of the true rate of errors that happen from the time a human biopsy specimen arrives in the anatomic pathology laboratory until the completed slides are ready to be diagnosed by a pathologist.
More Anatomic Pathology Labs Now Use Lean and Six Sigma
One such development is the growing acceptance and use of quality management methods, more specifically Lean, Six Sigma, and continuous improvement. These techniques help clinical laboratories do two things. First, in real time, the error rates (failure to meet specifications) for each process in the workflow can be measured with greater precision. Second, the external sources of error and systemic sources of failure for these work processes can be identified, thus enabling pathologists and histology lab staff to take corrective action.
The other development is the clinical use of by pathology groups of advanced technologies found in the latest generation of automated systems for processing tissue. These instrument systems eliminate manual steps in the process and—guided by sophisticated software—make it possible to individually handle each patient specimen in such a manner that the risk of cross-contamination is greatly reduced.
Studies in Peer-Reviewed Medical Laboratory Journals
Because of these developments, pathologists and clinical laboratory managers can expect to see more studies published in peer-reviewed medical laboratory journals that identify the error rates of long-standing histology work processes and also contrast those error rates with the performance of new automated histology systems.
In fact, one such study was published in recent months. It determined that batching slides and dunking them into the same stain bath in anatomic pathology laboratories may lead to cross-contamination of human biopsy specimens. This can sometimes produce false results. This study was sponsored by Ventana Medical Systems, Inc. and was published in the Journal of Histotechnology.
Stainer Bath Study Identified Errors in Tissue Processing
The study was called “Measurement of stainer bath contamination and evaluation of common mitigation strategies” and involved 69 surgical pathology laboratories worldwide operating a total of 72 stainers. The focus of the study was the process used for staining of tissues using hematoxylin and eosin (H&E). It was conducted by Angie Cahill, MBA, HT (ASCP), Area Support Manager, and Jeff Pearson, Senior International Product Manager, both employed by Ventana Medical Systems.
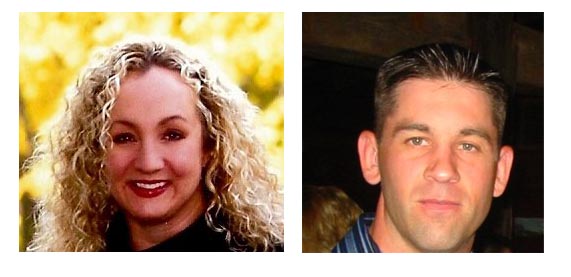
In their study titled “Measurement of stainer bath contamination and evaluation of common mitigation strategies,” which was published in the Journal of Histotechnology, authors (at left) Angie Cahill, HT(ASCP) and (at right) Jeff Pearson, both of Ventana Medical Systems, gathered data from 69 pathology laboratories. They found that each staining system used by the labs participating in the study produced extraneous tissue cross-contamination on the blank patient evaluation slides that were used in the study. (Photos copyright Cahill and Pearson, respectively.)
“Methods relative to the staining of tissues using hematoxylin and eosin (H&E) have largely not evolved beyond linear batch staining processes,” wrote Cahill and Pearson in the study abstract. “The batching of slides in the histopathology laboratory inherently leads to the sharing of the various reagents among those specimens being processed through the baths. This study assessed rates of extraneous tissue contamination found in selected stainer bath containers from the deparaffinization portion of the H&E linear staining procedure.”
To establish one baseline for their study, Cahill and Pearson called attention to the 1996 College of American Pathologists (CAP) Q-Probes study [Arch Pathol Lab Med. 1996;120:1009–14]. Authors Gephardt, Zarbo, and their coworkers “confirmed through prospective and retrospective studies the presence of extraneous tissue contaminants on patient slides,” wrote Cahill and Pearson.
Extraneous Tissue Found on 1,653 of 57,083 Slides in the Study
“The retrospective portion of their study included a population of 57,083 slides and considered the degree of extraneous tissue contamination and diagnostic difficulty,” they stated.” Extraneous tissue was present on 1,653 slides and severe diagnostic difficulty was demonstrated in 0.1% of the slides. Gephardt found that extraneous tissue contamination was indeed a defect in the linear slide staining process regardless of the outcome for the patient.”
When measured in terms of Six Sigma, the 1996 study by Gephardt and Zarbo—which included data from 275 pathology laboratories—determined that the stainer bath workflows in the participating labs produced cross-contaminated slides at the rate of 24,900 per one million events. Stated differently, the traditional stainer bath workflow performed at 3.5 Sigma. Alert readers of Dark Daily know that Six Sigma represents a process that only generates 3.4 defects per million events.
Extraneous Tissue Fragments Found on Blank Patient Simulator Slides
In their study, Cahill and Pearson determined that “this global, multi-laboratory study showed significant loss of extraneous tissue fragments from patient slides to stainer baths and tissue migration from the stainer baths onto blank patient simulator slides.” They further wrote that “the sharing of reagents during linear H&E staining contributed to a variable amount of tissue cross-contamination among simulated patient slides. Even though the level of contamination in the stainer baths differed, every participating laboratory showed evidence of tissue contamination, e.g. benign tissue fragments, as well as atypical and malignant fragments. The number of different tissue types in the baths ranged from 2 to 18, with an average of 8 per linear stainer.”
Other obvious variables did not come into play. “The magnitude of extraneous tissue cross-contamination, in terms of number of tissue types and total number of fragments found in the stainer baths, is independent of slide volume and reagent turnover in the stainer baths,” stated Cahill and Pearson. “That is, a small volume laboratory is just as likely to experience a high degree of tissue cross-contamination as a large volume laboratory. Similarly, how often laboratories changed or filtered reagents had no effect on the extraneous tissue contamination found in reagent baths. The study results indicate that stainer bath contamination is a random process.”
Pathologists Know and Use the Terms ‘Floaters’ and ‘Artifacts’
The findings of this study mirror what histologists and pathologists already know. The term in common use is “floaters” and describes the extraneous tissue contamination found in reagent baths. For the reasons listed above, pathology laboratories now have more sophisticated quality management tools and improved automated instrument systems that can be used to improve the quality and productivity of H&E staining of tissue specimens.
Because of the need to show constant improvement in patient safety, histotechnologists and pathologists can expect to see the bar raised regularly on the quality standards for the processing of human tissue. Moreover, because the regulatory infrastructure tends to lag market innovation, it can be expected that “best of class” pathology laboratories will be the leaders in moving the marketplace to a higher standard of care as it relates to how histology laboratories process tissue specimens.
—Patricia Kirk
Related Information:
Ventana CEO Headlines Congressional Briefing on Patient Safety and Cancer




Kudos, Angie & Jeff. The use of sophisticated quality management tools and automated instrument systems have improved the quality and productivity (including lower costs too) in the research / test labs thereby reducing the need to baby-sit the assays / experiments. Another step toward improving quality and value in the U.S. Health Care System, and beyond…..the “best of breed” pathology labs need not be apprehensive of any First-Mover Disadvantage: despite regulation lagging innovation, Market is clearly not.
Amarjit Jowandha
And, when they did get yeast infections, the condition cleared up faster. 3) Don’t use anti-bacterial soaps and detergents. Treating the symptoms isn’t effective unless you get to the cause and restore the body’s balance so that the infection doesn’t keep coming back.