News reports state that Anthem and Cigna have denied payment for some multigene panel tests, saying that the tests are unproven. Other insurers, such as UnitedHealthcare and Priority Health, pay for such tests but only for certain patients
A conflict is building between patients and health insurers over the reluctance among health plans to pay for new, expensive molecular diagnostic assays and genetic tests that clinical laboratory companies offer.
This conflict has caught the attention of the nation’s media. That is probably because it makes a great story, for example, to interview parents who can assert that their sick child suffered because their health insurance plan would not pay for a genetic test the parents believed would make a difference in their child’s clinical care. Of course, pathologists and medical laboratory professionals know that there are a significant number of expensive genetic tests being offered by various lab companies that lack extensive data to support their clinical efficacy.
Health Insurers Say Tests Are Unproven and Could Lead to Unneeded Care
In April, Reuters reported that Aetna, Anthem BlueCross BlueShield, and Cigna were denying payment for multigene panel tests. These insurers stated that the tests were unproven and could lead patients to seek care they don’t need. The nation’s largest health insurer, UnitedHealthcare, pays for such tests but only for certain patients, Reuters reported.
In a FierceHealthPayer article, Priority Health in Grand Rapids, Mich., said it would pay for comprehensive genetic testing of members diagnosed with aggressive forms of cancer.
Testing for breast cancer provides an example of how and why the rising number of genetic tests for this cancer is creating problems for payers. Earlier this year, Reuters reported that 17 genetics experts argued against testing for a wider panel of breast cancer-related gene mutations until the tests are proven to be valid and useful in clinical practice.
Paying for Genetic Tests If Results Don’t Change How Physicians Treat Patients
And, in another article earlier this month, Reuters reported that when genetic test results do not change how physicians manage a patient’s care, most experts agree that running such tests are not worth the cost and effort.
Nevertheless, clinical laboratories are offering multigene panels that test for abnormalities found in 25 or 29 genes for breast and ovarian cancer, Reuters stated. The new tests for breast cancer risk mutations go beyond the well-known BRCA genes and would offer actionable information for many women and their doctors, the news service reported.
Testing for this number of genes is new compared with most testing for women done since 2000. “For 15 years, at-risk women have only been tested for BRCA1 and 2,” Reuters reported.
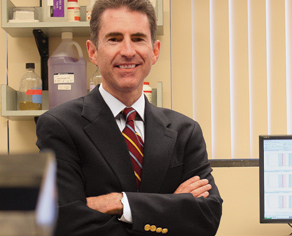
Leif W. Ellisen, M.D., Ph.D., Program Director for the Center for Breast Cancer at the Massachusetts General Hospital Cancer Center, is one of the authors of a study on multigene panels. In the study, the authors said, of multigene panels that such tests may identify 40% to 50% more individuals with hereditary cancer gene mutations than simply testing for BRCA1 or BRCA2, but determining whether such mutations would alter the clinical management of patients is unknown. (Photo copyright Massachusetts General Hospital.)
Genetic Testing for Some Cancers Is Evolving Rapidly Due to Multigene Panels
Leif W. Ellisen, M.D., Ph.D., Program Director for the Center for Breast Cancer at the Massachusetts General Hospital Cancer Center (MGH), told Reuters that even among genetics experts there is controversy over the utility of such testing. In addition to his work at MGH, Ellisen is a professor of medicine at the Harvard Medical School. He does not recommend widespread screening tests with multigene panels.
Ellisen is one of the authors of a study published Aug. 13, 2015, in JAMA Oncology about multigene testing. “The practice of genetic testing for hereditary breast and/or ovarian cancer (HBOC) is rapidly evolving owing to the recent introduction of multigene panels,” Ellisen and his co-authors wrote. “While these tests may identify 40% to 50% more individuals with hereditary cancer gene mutations than does testing for BRCA1/2 alone, whether finding such mutations will alter clinical management is unknown.”
In an editorial that accompanied this story in JAMA Oncology, Elizabeth M. Swisher, M.D., an Adjunct Professor in the Department of Medicine, Division of Medical Genetics at the University of Washington Medical Center in Seattle, explained that in the mid-1990s, genetics experts urged caution about doing widespread testing for BRCA1/2 gene abnormalities. Physicians and other clinicians should be cautious now with multigene panels, she added.
Cancer Experts Urge Caution about Wider Use of Multigene Panels
“Many cancer genetics experts have again urged caution, characterizing the use of multigene testing in the clinical setting as premature,” wrote Swisher. “Yet thousands of women and their physicians are ignoring this advice, ordering a wide selection of multiplex tests daily. The train has left the station and is unlikely to return. It is therefore critical that we assess the clinical utility of such testing.
“Multigene testing is rapidly becoming the norm for genetic cancer-risk assessment. We must continue to assess the effect of such testing on clinical care and patient experience and work to provide meaningful guidelines for cancer-preventive care for those with less common genetic findings,” she concluded.
By suggesting caution, Swisher and Ellisen echo what health insurers are saying. Just since last fall, the federal Centers for Medicare & Medicaid Services (CMS) has stopped paying for screening tests—even those important pharmacogenetic screening tests that the Food and Drug Administration (FDA) suggests physicians should order before prescribing certain medications, such as blood thinners, among others.
Genetic Testing Labs Need to Provide Evidence of Clinical Utility
By not paying for such tests, health insurers have taken a different stance toward new diagnostic assays than they did in the past. In the decade from 2001 to 2010, payers were more open to reimbursing for new tests because they recognized that these tests were part of the process of developing evidence of clinical utility.
What’s different today is that payers are overwhelmed by the thousands of proprietary molecular assays and genetic tests that clinical laboratories offer for a variety of cancers and other conditions. Therefore, if health insurers continue to deny payment for these genetic tests, one consequence may be to discourage research labs and biotech companies from developing new assays that could be clinically significant for patient care.
—Joseph Burns
Related Information:
Researchers Oppose Unvalidated Gene Panel Tests for Cancer Links
Priority Health to Cover Comprehensive Genetic Testing
Usefulness of Multigene Testing; Catching the Train That’s Left the Station
Testing for More Breast Cancer Genes Offers Useful Information



