This CMS pilot program is another opportunity for clinical laboratories to provide medical lab test services and collect specimens outside of traditional sites of healthcare services
Clinical laboratories and anatomic pathology groups are once again reminded to develop strategies that support the increasing number of physicians providing medical care in nontraditional outpatient settings. Now in its seventh year, the Medicare Independence at Home program is reviving the tradition of healthcare providers making house calls to elderly patients who have certain chronic illnesses, and so far, the results are promising.
Primary care teams at the 14 participating healthcare providers include physicians, nurse practitioners, physician assistants, pharmacists, social workers, and other staff.
Hospital networks participating in the federal Centers for Medicare and Medicaid Services (CMS) primary care pilot program are saving the government millions of dollars, while improving healthcare outcomes for their chronically ill patients and earning millions in return.
A CMS fact sheet states that to qualify for incentive payments, participating providers must meet performance thresholds of at least three of the following six measures:
- Follow-up contact within 48 hours of a hospital admission, hospital discharge, and emergency department visit;
- Medication reconciliation in the home within 48 hours of a hospital discharge and emergency department visit;
- Annual documentation of patient preferences;
- Hospital admissions for ambulatory care sensitive conditions; and
- Emergency department visits for ambulatory care sensitive conditions.
Northwell Health House Calls a Model of Success
The Independence at Home (IAH) demonstration project from the federal Center for Medicare and Medicaid Innovation (CMMI) was established in 2010 as part of the Affordable Care Act. In 2018, Congress extended the pilot for another two years and increased the number of eligible participants from 10,000 to 15,000.
Northwell Health House Calls has been a model of success within the federal IAH demonstration project. The New York-based healthcare provider has annually reduced costs while improving health outcomes for participating patients.

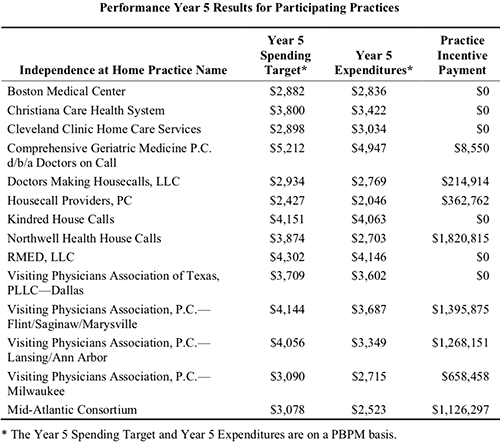
Results from the fifth year of the program (Oct. 1, 2016 through Sept. 30, 2017) show Northwell Health reduced per-beneficiary-per-month (PBPM) expenditures to $2,703, compared to a spending target of $3,874, according to the most recent CMS Fact Sheet. In return, Northwell Health received an incentive payment of more than $1.82 million. That’s the largest payout among the eight practices that met incentive payment quality benchmarks and savings requirements.
According to the news release, patients in Northwell’s House Calls program receive comprehensive, coordinated care, that includes ultrasounds, radiology, electrocardiograms, sleep studies, clinical laboratory work, physical exams, occupational and speech therapy, and social services, as well as intravenous fluids and prescription refills.
Physicians, nurse practitioners, and other clinicians are available for urgent, same-day visits during the work week. The team also is accessible 24/7 to answer clinical questions from patients and caregivers, or to arrange urgent services.
In an interview with Crain’s New York Business, Karen Abrashkin, MD, Medical Director of Northwell Health House Calls, said, “We’ve achieved cost savings by providing really good primary care and ongoing care for medical illnesses. We’re responsive to patients whenever they have a change in condition.”
How Patients Qualify for Medicare’s IAH Program
To qualify for the Independence at Home pilot, patients must:
- Currently be Medicare beneficiaries with two or more chronic health conditions;
- Need help with activities of daily living; and
- Have had a hospital admission and rehab stay within the past year.
Though he praises the House Calls program’s success, Kristofer Smith, MD, Senior Vice President of Population Health Management at Northwell Health stated that the program should be expanded slowly and only extended to those who would benefit most from in-home care.
“We need to be thoughtful about making sure we’re not expanding beyond the populations for whom we know it works because [it would] dilute the results,” he told Modern Healthcare.

Will Medicare’s Primary Care at Home Program Continue Beyond the Pilot?
The Independence at Home pilot is scheduled to end Dec. 31, 2020. What happens next is uncertain. Efforts in Congress to create a permanent home-based primary care program under Medicare have not yet gained traction despite bipartisan support.
Thomas Cornwell, MD, CEO, Home Centered Care Institute (HCCI), a national non-profit organization focused on advancing home-based primary care, is skeptical the primary care provider workforce could meet increased demand. He told Home Health Care News that question is “the greatest unknown.”
Nevertheless, the apparent success of Medicare’s Independence at Home pilot program should be a wakeup call to clinical laboratories and anatomic pathology groups that the trend of providing medical services in lower-cost settings will likely continue.
That means medical laboratory leaders should be developing strategies to support providers who are delivering medical care in nontraditional healthcare environments.
—Andrea Downing Peck
Related Information:
Independence at Home Demonstration Performance Year 5 Fact Sheet
Medical House Calls Program Improves Care, Reduces Costs of Treating Elderly Patients at Home
Northwell Wins Big in Medicare Pilot Home-Based Primary Care
Northwell Shows Savings in Medicare Testing House Calls
Elderly and Frail Patients Benefit from Receiving Care in the Comfort of Their Homes



