Clinical laboratories may see increase in flu and COVID-19 specimen processing as people return to pre-pandemic social behaviors, experts predict
While SARS-CoV-2 infections continue to ravage many parts of the world, influenza (flu) cases in North America have hit a historic low. As winter approached last year, infectious disease experts warned of a “twindemic” in which the COVID-19 outbreak would combine with seasonal influenza to overwhelm the healthcare system. But this did not happen, and many doctors and medical laboratory scientists are now investigating this unexpected, but welcomed, side-effect of the pandemic.
“Nobody has seen a flu season this low, ever,” said William Schaffner, MD, Professor of Preventive Medicine in the Department of Health Policy and Professor of Medicine in the Division of Infectious Diseases at Vanderbilt University School of Medicine in Nashville, in a report from WebMD, titled, “What Happened to Flu Season?”
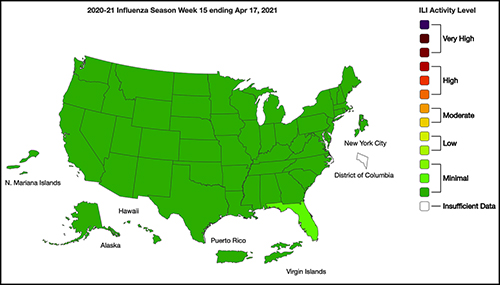
From the start of the current flu season in September 2020, clinical laboratories in the US reported that 1,766 specimens tested positive for flu out of 931,726—just 0.2%—according to the CDC’s Weekly US Influenza Surveillance Report. That compares with about 250,000 positive specimens out of 1.5 million tested in the 2019-2020 flu season, the CDC reported. Public health laboratories reported 243 positive specimens out of 438,098 tested.
Fear of COVID-19 Linked to Fewer Flu Deaths in Children
WebMD reported that just one child in the US has died from the flu this year, compared with 195 in 2020. Why the low numbers?
Speaking to WebMD, Isaac I. Bogoch, MD, Clinical Investigator, Toronto General Hospital Research Institute (TGHRI) and Infectious Diseases Consultant and General Internist at the Toronto General Hospital, cited three likely reasons:
- Precautions people take to avoid COVID-19 transmission, including masking, social distancing, and handwashing.
- Reduced human mobility, including less international travel.
- Higher-than-usual flu vaccination rates. As of February 26, the CDC reported that nearly 194 million doses of flu vaccine had been distributed in the US.
WebMD noted this could be a record, but that the CDC data doesn’t indicate how many doses were actually administered.
However, Schaffner told WebMD that efforts to keep kids home from school and away from social gatherings were likely a bigger factor. “Children are the great distributors of the influenza virus in our society,” he said. But due to fears about COVID-19 transmission, kids “weren’t even playing together, because mothers were keeping them off the playground and not having play dates.”
Repercussions for Fighting Flu Next Year
Public health experts welcomed the low flu levels, however, Politico reported that limited data about flu circulation this year could hamper efforts to develop an effective vaccine for next season’s flu strains.
“We may have a combination of low public health measures at the population level with a low effectiveness vaccine,” Lawrence Gostin, JD, University Professor at Georgetown University, told Politico. “And then, so you might have a raging flu season next year.” Gostin leads the O’Neill Institute for National and Global Health Law and serves as Director of the World Health Organization’s Collaborating Center on National and Global Health Law.
Each February, Politico explained, experts convened by the World Health Organization (WHO) look at data from the current and previous flu seasons to predict which strains are likely to predominate in the Northern Hemisphere next winter. That includes data about which strains are currently circulating in the Southern Hemisphere. The WHO uses these predictions to recommend the composition of flu vaccines. In the US, the final decision is made by an FDA advisory committee.
A similar WHO meeting in September guides vaccine development in the Southern Hemisphere.
The WHO issued this year’s Northern Hemisphere recommendations on Feb. 26. The advisory includes recommendations for egg-based and cell- or recombinant-based vaccines, and for quadrivalent (four-strain) or trivalent (three-strain) vaccines.
In a document accompanying the recommendations, the WHO acknowledged concerns about this year’s limited pool of data.
“The volume of data available from recently circulating influenza viruses, and the geographic representation, have been significantly lower for this northern hemisphere vaccine recommendation meeting than is typical,” the document stated. “The reduced number of viruses available for characterization raises uncertainties regarding the full extent of the genetic and antigenic diversity of circulating influenza viruses and those likely to pose a threat in forthcoming seasons.”
The report notes that experts identified changes in circulating Influenza A(H3N2) viruses this year, and that the changes are reflected in the new vaccine recommendation.
But Paul A. Offit, MD, who serves on the FDA’s vaccine advisory panel, downplayed worries about the vaccine. “The belief is that there was enough circulating virus to be able to pick what is likely to be the strains that are associated with next year’s flu outbreak,” he told Politico. Offit is a Professor of Vaccinology and Pediatrics at the Perelman School of Medicine at the University of Pennsylvania and Director of the Vaccine Education Center at the Children’s Hospital of Philadelphia.

Offit suggests that efforts to mitigate the COVID-19 outbreak could be useful to combat other infectious disease outbreaks. However, both Offit and Gostin expressed doubt about that prospect.
“I mean, could we reasonably in a winter month, wear masks just at least when we’re outside in large crowds? … Or are we comfortable having hundreds of 1000s of cases of hospitalizations for flu and 10s of 1000s [of] deaths? I suspect the answer is B. We’re comfortable with that, we’re willing to have that even though we just learned, there’s a way to prevent it,” Offit told Politico.
“Remember after the 1918 flu pandemic, most people don’t realize what happened when that was over. But what happened was the roaring ‘20s,” Gostin told Politico. “People started congregating, mingling, hugging, kissing. All the things they missed. They crowded into theaters and stadiums and went back to church. That’s what’s likely to happen this fall and that makes the influenza virus very happy.”
So, what should clinical laboratories expect in future flu and COVID-19 vaccines? That is not yet clear. One thing is certain, though. New lab test panels that test for influenza and the SARS-CoV-2 coronavirus will be arriving in the marketplace.
—Stephen Beale
Related Information:
Fears of ‘Twindemic’ Recede as US Influenza Rates Stay Low
The Mystery of the Flu-COVID ‘Twindemic’ That Never Happened
The Pandemic Dramatically Reduced Flu Cases. That Could Backfire.
Weekly U.S. Influenza Surveillance Report
For mRNA Vaccines, COVID-19 Is Just the Beginning
How COVID Unlocked the Power of RNA Vaccines
Coronavirus Vaccine Technology Is Paving the Way for a Whole New Approach to Flu Shots
Duke Researchers Working on mRNA Flu Vaccine That Would Last Up to 5 Years



