Clinical laboratories are being squeezed on both sides as rising healthcare costs affect their patients while increasing health plan costs impact their employees’ health coverage
When UnitedHealthcare CEO Brian Thompson was murdered on Dec. 4, the nation’s attention focused on the negative impact ever-increasing costs of healthcare coverage is having on the average American. Clinical laboratories and anatomic pathology groups experience this trend firsthand as annual increases in the cost of health plans affect their employees.
To understand just how raw the public is feeling about health insurance, consider that in a recent Emerson College poll, 41% of respondents ages 18-29 stated that Thompson’s murder was “completely” or “somewhat” acceptable.
While the majority of the country believes that such violence is not an acceptable way to solve one’s problems, the message is clear that Americans’ waning trust in health insurance companies has reached unhealthy levels.
“Health insurance costs are far outpacing inflation, leaving more consumers on the hook each year for thousands of dollars in out-of-pocket expenses. At the same time, some insurers are rejecting nearly one in five claims. That double whammy is leaving Americans paying more for coverage yet sometimes feeling like they’re getting less in return,” CBS News reported.
Twenty-five years of increases from the insurance industry make it clear why the relationships between healthcare consumers and insurance companies has soured.
“Employers are shelling out the equivalent of buying an economy car for every worker every year to pay for family coverage,” said Kaiser Family Foundation President and CEO Drew Altman (above) in a news release. “In the tight labor market in recent years, they have not been able to continue offloading costs onto workers who are already struggling with healthcare bills.” Clinical laboratories and pathology groups are among those employers struggling to provide affordable health coverage for their employees. (Photo copyright. Kaiser Family Foundation.)
People Are Frustrated
The cost of living in America has risen dramatically in the past decade. So much so that people are increasingly becoming frustrated and lashing out against companies that appear to be making record profits while their customers struggle to pay for their products and services.
A recent Kaiser Family Foundation (KFF) Health Tracking Poll found that “About one in five adults (19%) say they have difficulty affording their bills each month and about four in 10 (37%) say they are just able to afford their bills each month, while a little over four in 10 (44%) say they are both able to pay their bills and have some money left over.”
Simultaneously, according to KFF, “Employees’ share of their [health insurance] premiums are also on the rise, with a worker with family coverage typically paying premiums of $5,700 per year in 2017, the most recent year for that data, up from about $1,600 in 2000. … The average family deductible—the amount paid out-of-pocket before insurance kicks in—has increased from $2,500 in 2013 to $3,700 in 2023.”
This double-whammy in costs has a growing number of American’s worrying about unexpected healthcare bills and the overall cost of keeping their families adequately covered for the future.
“We’ve gotten to a point where healthcare is so inaccessible and unaffordable, people are justified in their frustrations,” said Céline Gounder, MD, a CBS News medical contributor and editor-at-large for public health at KFF Health News.
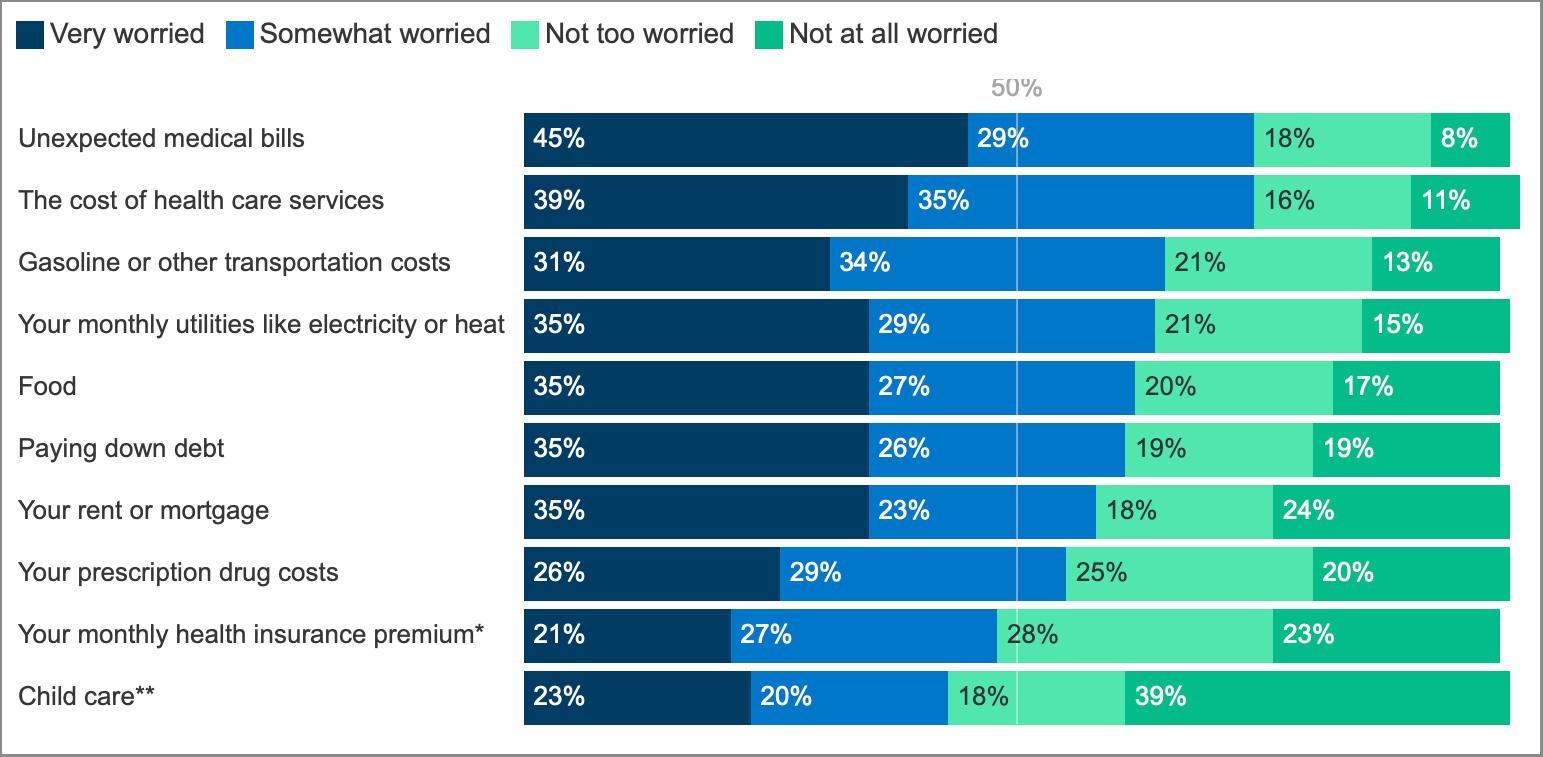
The chart above taken from a KFF Health Tracking Poll (Jan. 30-Feb. 7, 2024) shows participants’ answers when asked, “How worried, if at all, are you about being able to afford each of the following for you and your family?” Results indicate, according to KFF, that three in four people polled are worried about paying future healthcare bills and covering increasing insurance costs. (Graphic copyright: KFF.)
AI and Coverage Denials
Coverage denials is another sore spot for many people, impacting nearly one in five claims in nongroup qualified health plans in 2021, KFF found. This ranged from 2% to 49% depending on the company.
“When you are paying for something, they don’t give it to you, and they keep raising prices … you will be frustrated by that,” Holden Karau, a software engineer and creator of Fight Health Insurance, a free online service that helps people appeal their denials, told CBS News. Karau’s company uses artificial intelligence (AI) to help customers create appeal letters.
But the use of AI in healthcare coverage has also drawn criticism. Insurance companies are increasingly using AI to review claims and issue denials, and the lack of transparency has led to lawsuits. Last year, CBS News covered lawsuits brought by the families of two deceased individuals who accused UnitedHealthcare of “knowingly” using a “faulty” AI algorithm to deny the patients medically necessary treatments.
Karau noted, “With AI tools on the insurance side, they have very little negative consequences for denying procedures,” CBS News reported. “We are seeing really high denial rates triggered by AI. And on the patient and provider side, they don’t have the tools to fight back,” she added.
“Unhappiness with insurers stems from two things: ‘I’m sick and I’m getting hassled,’ and the second is very much cost—‘I’m paying more than I used to, and I’m paying more than my wages went up,’” Rob Andrews, CEO of Health Transformation Alliance, a company that helps healthcare providers and other self-insured companies improve coverage for their employees, told CBS News. “A lot of people think they are getting less,” he added.
Effects on Clinical Laboratories
Even as individuals and families pay more money each year in healthcare premiums, deductibles, and out-of-pocket expenses, clinical laboratories have seen payers cut reimbursement for many lab tests. Thus, labs are dealing with a double-squeeze on their finances. On the income side, reimbursement for tests is under pressure, while on the cost side, the cost of health benefits for employees climbs annually.
Clinical lab and pathology managers will want to stay aware of these trends and take advantage of any opportunity to lower costs and pass on those savings to their patients.
—Kristin Althea O’Connor
Related Information:
As Anger at UnitedHealthcare Boils Over, Americans Pay More than Ever for Health Insurance
Why Americans Are Outraged Over Health Insurance—and What Could Change


