Apr 2, 2018 | Digital Pathology, Laboratory Instruments & Laboratory Equipment, Laboratory Management and Operations, Laboratory News, Laboratory Operations, Laboratory Pathology, Laboratory Testing
Ever shrinking “lab-on-a-…” technologies, a boon to medical laboratories and anatomic pathologists in remote resource-strapped regions, also have a place in modern labs
Researchers took another leap forward in reducing the size of clinical laboratory diagnostic tests and observational tools. This demonstration involved lab-on-a-fiber technology and showed promise in both monitoring anatomic pathology biomarkers in vivo and supplementing the abilities of existing lab-on-a-chip and microfluidic devices.
Lab-on-a-Fiber Next Technological Step Toward Miniaturization
In 2013, Dark Daily reported on research into an implantable laboratory-on-a-chip (LOC) for monitoring blood chemistry during chemotherapy. It was a major breakthrough at the time, which promised new and powerful tools for cancer treatment regimens.
However, most LOC systems aren’t designed for wet environments. Also, while microfluidics and flexible membranes allow for smaller footprints and tighter placement, they are still invasive in ways that might make patients uncomfortable or make real-world use less than ideal. And, long-term use brings further complications, such as corrosion or foreign-body granulomas.
Thus, lab-on-a-fiber’s ability to function in vivo, is one of the device’s principal advantages, as ExtremeTech noted.
Lab-on-a-fiber technology addresses many concerns. It is small enough to insert directly into organs, muscle mass, or veins when used as biosensors. And the fibers can return a wealth of information by using light and reflection, while allowing for minimal discomfort and precision placement.
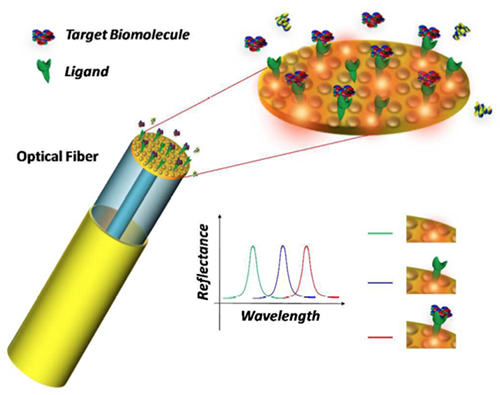
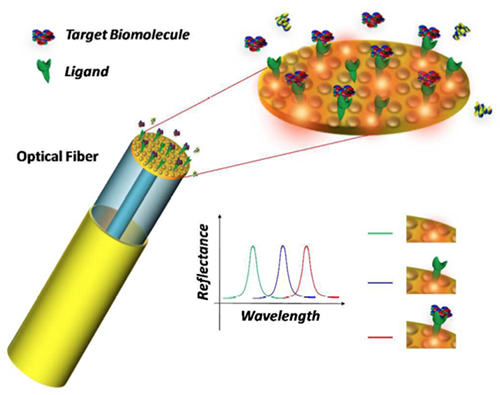
Schematic of the lab-on-a-fiber biosensing principle. A metallic nanostructure supporting a resonant plasmonic mode is integrated on the optical fiber tip. When a molecular binding event occurs at the sensor surface, the reflectance peak associated to the plasmonic mode shifts towards longer wavelengths. (Image and caption copyright: Analyst/The Royal Society of Chemistry.)
The Past and Future of Scaling Clinical Laboratory Testing
Dark Daily has followed these miniaturization trends for years starting with their earliest stages. A detailed timeline of developments can be viewed in “Lab-on-a-Chip Diagnostics: When Will Clinical Laboratories See the Revolution?” from 2016.
Additional Dark Daily “lab-on-a-…” coverage includes:
- IBM Watson Health and Mount Sinai Health System team up to use LOC solutions to separate biomolecules as small as 20nm from samples (See Dark Daily, “IBM and Mount Sinai Researchers Develop Innovative Medical Lab-on-a-Chip Solution,” October 3, 2016); and,
- Lab-on-Skin devices for monitoring biomarkers and electrophysiological signals, providing human-machine interfaces, and facilitating optogenetics (See Dark Daily, “In the Field of Nano-Scale Diagnostics, Many Researchers Are Developing ‘Lab-on-Skin’ Technologies That Can Monitor Many Clinical Laboratory Biomarkers,” January 15, 2015).
In the past year, a myriad of lab-on-a-fiber applications also have received media coverage, including:
Developers believe lab-on-a-fiber approaches could offer further adaptability and functionality to other “lab-on-a-…” technologies. For example, as highlighted in Advanced Science News, researchers are employing lab-on-a-fiber technologies to further refine and improve LOC functions and designs.
“As the scientific world moves inexorably to smaller dimensions … The emerging concept of ‘lab‐on‐fiber’ will give the optical fiber platform additional (highly integrated) functionalities,” noted Deepak Uttamchandani, PhD, Vice Dean Research, Faculty of Engineering, and, Robert Blue, PhD, Research Fellow, both at the University of Strathclyde, Glasgow, UK, in their review paper, “Recent Advances In Optical Fiber Devices for Microfluidics Integration.” The paper, published in the Journal of Biophotonics, examined “the recent emergence of miniaturized optical fiber-based sensing and actuating devices that have been successfully integrated into fluidic microchannels that are part of microfluidic and lab‐on‐chip systems.”

In his review paper on the emerging concept of lab-on-a-fiber, Deepak Uttamchandani, PhD, notes, “The versatility of the optical fiber platform has already allowed researchers to conduct immunoassays in microchannels using both fluorescently‐labelled and label‐free formats whilst gaining advantages of reduced assay time and increased sensitivity.” (Photo copyright: University of Strathclyde.)
Lab-on-a-Fiber: Another Step Forward or a Major Change?
At each milestone in the scaling of clinical laboratory testing, experts and media outlets predicted the demise of big laboratories and the dawn of a POC-centric testing era. Yet, despite 20-plus years of progress, this has yet to happen.
While it is critical for anatomical pathology leaders and clinical laboratory managers to stay abreast of developments in testing technology, much of the innovation behind lab-on-a-fiber remains strictly in the research realm. Challenges to the commercialization of these new techniques include both physical factors, such as design and manufacture of ready-to-use tests, and regulatory concerns, including FDA clearances and payer approval of new assays and diagnostic procedures.
Until researchers and test manufacturers overcome these hurdles, threats to current standards and workflows are minimal. However, much like the gains in scale realized through incorporating lab-on-a-chip concepts into clinical laboratory testing, the research powering these innovations might prove useful in further improving and expanding medical laboratory testing options.
—Jon Stone
Related Information:
Optical Fiber Devices for Microfluidics Integration Open Up New Horizons for Advanced “Lab-on-a-Chip” Technologies
Recent Advances in Optical Fiber Devices for Microfluidics Integration
Lab-on-Fiber Technology: A New Vision for Chemical and Biological Sensing [Abstract]
Lab-on-Fiber Technology: A New Vision for Chemical and Biological Sensing [Full Downloadable PDF]
How We’re Shrinking Chemical Labs onto Optical Fibers
Lab-on-Fiber Could Shine Light on Disease
Doctors Might Soon Diagnose You by Feeding a Lab-on-a-Fiber Straight into Your Veins
Fiber-Optic Device Can Detect Stray Cancer Cells and Improve Tumor Removal: Study
Fiber Optic Probe Beats a Biopsy for Measuring Muscle Health
Lab-on-a-Chip Diagnostics: When Will Clinical Laboratories See the Revolution?
Implantable Medical Laboratory-on-a-Chip Continuously Monitors Key Chemicals in Chemotherapy and High-Risk Patients
In the Field of Nano-Scale Diagnostics, Many Researchers Are Developing ‘Lab-on-Skin’ Technologies That Can Monitor Many Clinical Laboratory Biomarkers
Hematology on a Chip: University of Southampton Develops POC Blood Analysis
Sleek ‘Lab in a Needle’ Is an All-in-One Device That Detects Liver Toxicity in Minutes during a Study, Showing Potential to Supplant Some Medical Laboratory Tests
Whole Animal Assays Use Lab-on-a-Chip at MIT
IBM and Mount Sinai Researchers Develop Innovative Medical Lab-on-a-Chip Solution
In the Field of Nano-Scale Diagnostics, Many Researchers Are Developing ‘Lab-on-Skin’ Technologies That Can Monitor Many Clinical Laboratory Biomarkers
Mar 30, 2018 | Compliance, Legal, and Malpractice, Digital Pathology, Instruments & Equipment, Laboratory Management and Operations, Laboratory News, Laboratory Operations, Laboratory Pathology, Laboratory Testing, Management & Operations
Developers believe participants will be interested in controlling how their private health data is provided to medical laboratories, drug companies, research organizations, and the federal government, while also earning an income
Bitcoins for blood tests, anyone? A new venture is examining the idea of exchanging cryptocurrency, a digital asset, for the results of weekly clinical laboratory tests and photographs of body parts from healthcare consumers. If successful, in a couple of years, people might be able to earn a “basic income” from selling their private health data to pharmaceutical companies, medical laboratories, research organizations, the federal government, and more.
Insilico Medicine, a Baltimore developer of artificial intelligence (AI) solutions for research and pharmaceutical companies, and the Bitfury Group, a blockchain technology company based in Amsterdam, Holland, are working together on the project they call Longenesis, a blockchain-based platform that uses AI to collect, store, manage, and trade data, such as medical records and health data.
Marketing Human Life Data
The two participants presented their novel idea this past November in Taipei, Taiwan, at the TaiwanChain Blockchain Summit. They published their report in Oncotarget, an open-access biomedical journal that covers oncology research. The authors of the paper believe blockchain and AI technologies could support patients and physicians in working with medical data.
“There are many companies engaged in the marketplaces of human life data with billions of dollars in turnover. However, the advances in AI and blockchain allow returning the control of this data back to the individual and make this data useful in the many new ways,” Alex Zhavoronkov, PhD, founder of Insilico Medicine, told Cryptovest.
“I would love to live in a world where I’m motivated to regularly take all kinds of medical tests for free, I get the data back, and I will be able to sell this data to the marketplace, and I earn all kinds of goods and services—primarily health related,” Zhavoronkov told Motherboard.

Alexander Zhavoronkov, PhD, Founder and CEO of Insilico Medicine, told Motherboard, “Right now, it’s difficult to predict. But I think that if [users] submit blood tests, pictures, transcriptomes let’s say on a weekly basis, you probably will be able to earn a good universal basic income.” Zhavoronkov is describing a new business model involving clinical laboratory testing. (Photo copyright: Insilico Medicine.)
Combining blockchain and AI technologies is one of the many emerging technological advances emerging to enhance the medical and pharmaceutical industries.
“Recent advances in machine intelligence turned almost every data into health data. The many data types can now be combined in the new ways: one data type can be inferred from another data type and systems learning to optimize the lifestyle for the desired health trajectory can now be developed using the very basic and abundant data,” noted Polina Mamoshina, research scientist at Pharma AI, a division of Insilico Medicine, during the company’s presentation at TaiwanChain. “Pollen, weather, and other data about the environment can now be combined with the human biomarkers to uncover and minimize the allergic response among the myriad of examples. People should be able to take control over this data.”
Because pharmaceutical companies rely on data mining to obtain individual demographic information and medical records, the growth potential for this type of product is huge.
Clinical Laboratory Test Results Earn LifePound Tokens
Longenesis is still being tested, but Zhavoronkov hopes it will be ready for the public within the next two years. The plan is to utilize blockchain technology to collect and store patient medical data in exchange for their cryptocurrency, known as LifePound.
According to the Longenesis website, “Longenesis is a marketplace, which uses personal health data, transformed into a LifePound token. LifePound is used inside a marketplace as a monetary system, powered by Exonum blockchain technology to keep data secure and transparent. Tokens are distributed between Longenesis marketplace members and are used for transactions between the following elements:
- Developers;
- Users;
- Data providers;
- Customers; and the,
- Stock cryptocurrency market.
The developers believe the “Longenesis Data Marketplace will be able to provide new insights in the fields of healthcare research and development. It will provide analysis and recommendations to pharmaceutical companies to help develop new drugs.”
It’s too early to predict whether Longenesis will be successful and catch on with the public. However, the popularity of cryptocurrency, and the opportunity to earn an income from one’s clinical laboratory data, could encourage individuals to participate in this type of endeavor.
In addition, this is a highly unusual and unexpected approach to encourage consumers to undergo regular medical laboratory testing in order to earn payment by a digital currency. It is a reminder of how rapid advances in a myriad of technologies are going to make it possible for entrepreneurs to create new business models that involve clinical laboratory tests and the data produced by such tests.
—JP Schlingman
Related Information:
This Biotech Company Wants You to Give It Selfies and Blood Tests in Exchange for Cryptocurrency
A Decentralized Medical Record Marketplace Powered by Human Data
Blockchain, AI Could Spur Biomedical Research, Insilico Medicine Says
Converging Blockchain and Next-generation Artificial Intelligence Technologies to Decentralize and Accelerate Biomedical Research and Healthcare
Blockchain, Explained
Mar 21, 2018 | Digital Pathology, Instruments & Equipment, Laboratory Instruments & Laboratory Equipment, Laboratory Management and Operations, Laboratory News, Laboratory Operations, Laboratory Pathology, Laboratory Sales and Marketing, Laboratory Testing, News From Dark Daily
January’s press release confirmed the tech company is working to integrate critical medical data into its mobile devices, while further promoting interoperability and patient access
While interoperability has improved since the earliest electronic health record (EHR) systems, today’s active patients often need to sort through multiple healthcare portals—including those of clinical laboratories and anatomic pathology groups—to get a comprehensive view of their medical history. Not only can this be time consuming, but also inconvenient if the patient lacks access to a computer.
Thus, it’s no surprise that in a January 24 press release, mobile technology giant Apple announced plans to enter the development ring and create an improved EHR for its mobile device users by updating its existing “Health” mobile application (app). The iOS 11.3 update, among other things, is designed to enable Apple iPhone owners to receive critical medical data, such as medical laboratory test results, directly on their devices.
“Our goal is to help consumers live a better day. We’ve worked closely with the health community to create an experience everyone has wanted for years—to view medical records easily and securely right on your iPhone,” said Apple COO Jeff Williams in the press release.
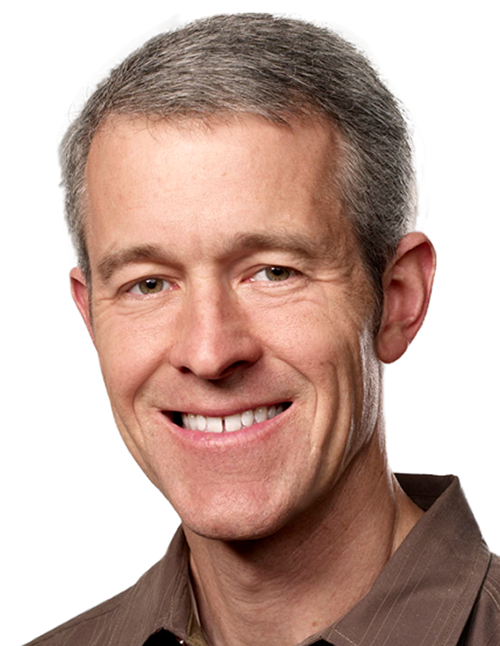
Jeff Williams (above), COO at Apple, notes that, “By empowering customers to see their overall health, we hope to help consumers better understand their health and help them lead healthier lives.” (Photo copyright: Apple.)
The new features are already available to developers in the latest iOS 11.3 beta 3 release. However, release to the public is expected soon with the issuance of the iOS 11.3 final release. This means that patients will not need to download extra apps—or remember to use them—to take advantage of the feature.
New Way to Improve Patients’ Access to Health Data or Just Another Data Silo?
The Apple Health Records platform adheres to Fast Healthcare Interoperability Resources (FHIR) protocols for transmission of data. Providers send information to Apple which then aggregates the information, transmits it to patients’ iPhones and notifies them of the updates.
All information stored on the device is encrypted in storage and protected from unauthorized access by the user’s password.
Through the new Health Records interface, users view this aggregated data as a timeline, conduct searches, and share information with other parties as they deem appropriate.
Current medical information listed in the press release includes:
- Allergies;
- Conditions;
- Immunizations;
- Clinical laboratory results;
- Medications;
- Procedures; and,
- Vitals.
Currently, the platform integrates data from three major EHR developers:
- Epic;
- Cerner; and,
- AthenaHealth

Apple’s update to the Health app makes it easier for people to access and control of all of their health records and data. This included medical laboratory tests. (Image and caption copyright: Apple.)
Apple is also working with 12 health institutions across the US in the first phase of the project, including:
In the Apple press release, Stephanie Reel, CIO at John Hopkins Medicine in Baltimore, stated, “Streamlining information sharing between patients and their caregivers can go a long way towards making the patient experience a positive one. This is why we are excited about working with Apple to make accessing secure medical records from an iPhone as simple for a patient as checking email.”
Previous Attempts at Mobile Health Record Devices Got Mixed Results
This isn’t the first time a major technology company has attempted to enter the mobile health market. Google Health was shuttered in 2011 citing low adoption. Wearable fitness trackers, such as Fitbit (NYSE:FIT) enjoyed a bubble, but are now seeing mixed success in terms of long-term adoption and use, according to The Motley Fool. More to the point, they’ve never quite become the holy grail of monitoring and data collection that some experts predicted, Huffington Post reported.
However, Apple’s investments and interest in healthcare-related technologies has led to wide speculation that they would enter the health market this year. (See Dark Daily “Apple May Be Developing Mobile Device Technology to Monitor User’s Health and Transmit Data in Real Time.”)
Larry Dignan, Editor-in-Chief at ZDNet, builds a compelling case for why this could be the attempt that succeeds in providing a consolidated platform for clinical laboratories, physicians, and other care providers to push data directly to patients and—with the patient’s permission—to each other, regardless of the platforms healthcare facilities use to store and transmit data.
He notes that much of Apple’s newest features build on foundations laid by the healthcare industry to create scalable, functional EHR systems. By working with existing protocols, Apple’s Health Records platform is already positioned for compatibility with many healthcare providers.
Furthermore, Apple is already known for partnering at the enterprise level with major businesses and industries, while also holding the trust of millions of Americans who store their personal information on Apple devices.
Is Apple the Future of EHRs?
Despite this, until the platform—and adoption by the public—is proven a success, it will be yet another walled garden of medical information. Even then, Apple is only one segment of the global mobile market.
Unless Apple provides access to other platforms (such as Android), those patients—and the medical communities serving them—are left consolidating information on their own through a sprawl of various portals. This also means that medical laboratories, pathology groups, and other service providers must continue to invest time and funding into communicating data in ways compatible with a plethora of internal and external systems and software.
Still, the platform offers an intriguing glimpse at the future of medical records and heralds a shift toward empowering patients with easy, comprehensive access to their own data, which would be a boon to the medical laboratory industry.
—Jon Stone
Related Information:
Apple Previews iOS 11.3
Apple Announces Effortless Solution Bringing Health Records to iPhone
With Medical Records Tools, Apple Wades Deeper into Digital Health
Apple Confirms “Health Records” Solution with Aim to Bring Medical Records to iPhone
Apple Will Let You Keep Your Medical Records on Your iPhone
Apple Unveils mHealth Integration with EMR Data through Health App
Apple, Inc. Wants to Solve the Problem of Electronic Health Records
Viewpoint: How Realistic Is Apple’s Attempt at the EHR Industry? Very—6 Reasons Why
Apple Can Win Electronic Medical Record Game with Health Records in iOS 11.3: Here’s 7 Reasons Why
Apple Is Officially in the EHR Business. Now What?
Apple to Launch Health Records App with HL7’s FHIR Specifications at 12 Hospitals
Could Amazon or Apple Actually Make a Dent in the EHR Market?
Apple May Be Developing Mobile Device Technology to Monitor User’s Health and Transmit Data in Real Time
Mar 16, 2018 | Digital Pathology, Laboratory News, Laboratory Pathology, Laboratory Testing
Exercise contributes to improving the human microbiome in ways that fight disease and clinical labs might eventually provide tests that help track beneficial changes in a patient’s microbiome
With growing regularity, new discoveries about the human Microbiome have been reported in scientific journals and the media. Some of these discoveries have led to innovations in clinical laboratory tests over the past few years. Dark Daily reported on these breakthroughs, which include: improved cancer drugs, life extension, personalized medical treatments (AKA, precision medicine), genetic databases, and women’s health.
Now, a study from the University of Illinois at Urbana-Champaign (UI) has linked exercise to beneficial changes in the makeup of human microbiota. The researchers identified significant differences in the gut bacteria of obese and lean individuals who underwent the same endurance training. The lean individuals developed healthy gut bacteria at a much higher rate than the obese participants. And they retained it, so long as the exercise continued.
Thus, researchers believe weight loss and regular exercise could become critical components of new treatment regimens for many chronic diseases, including cancer.
Regular Exercise Increases Good Gut Bacteria in Humans and Mice
The UI researchers published the results of their study in Medicine and Science in Sports and Exercise, a journal of the American College of Sports Medicine. To perform their study, they analyzed the impact six weeks of endurance training had on the gut bacteria of 32 adults:
- Eighteen of the subjects were lean and the remaining 14 were obese;
- Eleven of the obese and nine of the lean participants were female; and,
- All 32 were sedentary before the study began.
The subjects participated in six weeks of supervised exercise three days/week. They started at 30-minutes/day and progressed to 60-minutes/day. Fecal samples were collected from the participants before and after the six weeks of training. The subjects were instructed to not change any of their dietary habits during the study.
Upon completion of the initial six-week exercise program, participants returned to a sedentary lifestyle for another six weeks and then researchers took more fecal samples.
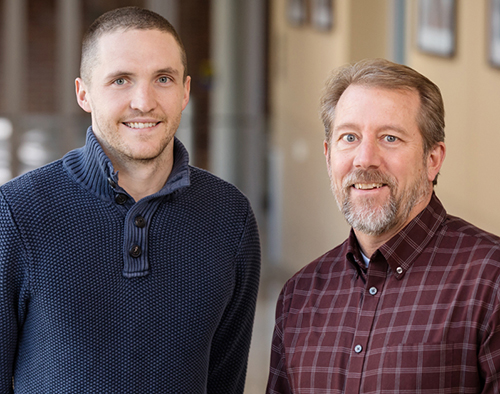
In a University of Illinois study, Jacob Allen, PhD-Candidate (left), and Jeffrey Woods, PhD (right), et al, concluded that regular exercise increased production of beneficial gut bacterial (microbiome) more in lean individuals than in obese participants. This finding could alter how anatomic pathologists and medical laboratories view exercise and weight loss for patients undergoing treatment regimens for chronic diseases. (Photo copyright: University of Illinois/L. Brian Stauffer.)
As a result of the study, the researchers found the gut bacteria of the subjects did change, however, those changes varied among the participants. Fecal concentrations of short chain fatty acids (SCFAs), particularly butyrate, increased in the guts of the lean participants but not in the guts of the obese subjects.
SCFAs have been shown to improve metabolism and reduce inflammation in the body, and they are the main source of energy for the cells lining the colon. However, nearly all of the beneficial changes in the participants’ gut bacteria disappeared after six weeks of non-exercise.
“The bottom line is that there are clear differences in how the microbiome of somebody who is obese versus somebody who is lean responds to exercise,” Jeffrey Woods, PhD, Professor, Department of Kinesiology and Community Health, College of Applied Health Sciences, University of Illinois at Urbana-Champaign and co-leader of the study, told UI’s News Bureau. “These are the first studies to show that exercise can have an effect on your gut independent of diet or other factors.”
Reduced Inflammation Promotes Healing
The researchers had previously performed a related study using lab mice and found similar results. For that experiment, mice were separated into two groups where some were permitted to run around and be active while the others were sedentary. The gut material from all of the mice was then transplanted into gnotobiotic (germ-free) mice where their microbiomes were exposed to a substance that was known to cause irritation and inflammation in the colon. The animals with the gut bugs from the active mice experienced less inflammation and were better than the sedentary mice at resisting and healing tissue damage.
“We found that the animals that received the exercised microbiota had an attenuated response to a colitis-inducing chemical,” Jacob Allen, PhD Candidate, co-leader of the study and former doctoral student at UI, now a postdoctoral researcher at Nationwide Children’s Hospital in Columbus, Ohio, told the UI News Bureau. “There was a reduction in inflammation and an increase in the regenerative molecules that promote a faster recovery.”
Exercise Added to Growing List of Benefits from Health Gut Bacteria
Similar research in the past has found that healthy gut bacteria may have many positive effects on the body, including:
- Improved immune health;
- Improved mood and mental health;
- Boosting energy levels;
- Improved cholesterol levels;
- Regulated hormone levels;
- Reduction of yeast infections;
- Healthy weight support;
- Improved oral health; and,
- Increased life expectancy.
Other ways to improve gut bacteria include: dietary changes, taking probiotics, lowering stress levels, and getting enough sleep. Now regular exercise can be added to this growing list.
Once further research confirms the findings of this study and useful therapies are developed from this knowledge, clinical laboratories should be able to provide microbiome testing that would help physicians and patients track the benefits of exercise on enhancing gut bacteria.
—JP Schlingman
Related Information:
Exercise Alters Our Microbiome. Is That One Reason It’s So Good for Us?
Exercise Training-induced Modification of the Gut Microbiota Persists After Microbiota Colonization and Attenuates the Response to Chemically-induced Colitis in Gnotobiotic Mice
Exercise Alters Gut Microbiota Composition and Function in Lean and Obese Humans
Exercise Changes Gut Microbial Composition Independent of Diet, Team Reports
Exercise Can Beneficially Alter the Composition of Your Gut Microbiome
Researchers Discover Link between Gut Bacteria and the Effectiveness of Certain Cancer Drugs; Knowledge May Lead to New Types of Clinical Laboratory Tests
Researchers in Two Separate Studies Discover Gut Microbiome Can Affect Efficacy of Certain Cancer Drugs; Will Findings Lead to a New Clinical Laboratory Test?
Attention Microbiologists and Medical Laboratory Scientists: New Research Suggests an Organism’s Microbiome Might Be a Factor in Longer, More Active Lives
Get the Poop on Organisms Living in Your Gut with a New Consumer Laboratory Test Offered by American Gut and uBiome
Mayo Clinic and Whole Biome Announce Collaboration to Research the Role of the Human Microbiome in Women’s Diseases Using Unique Medical Laboratory Tests
Feb 12, 2018 | Digital Pathology, Instruments & Equipment, Laboratory Management and Operations, Laboratory News, Laboratory Operations, Laboratory Pathology, Laboratory Testing
Doctors’ advocacy organization praises potential of ‘My Health Record’ but voices concerns about functionality, interoperability, and added burden placed on providers
Australia’s goal of implementing a nationwide electronic health record (EHR) system received a major boost when the country’s largest pathology laboratories signed agreements with the Australian Digital Health Agency (ADHA) to join the project. But the My Health Record system has yet to fully win over providers as the Australian Medical Association (AMA) raises concerns over functionality, interoperability, and the added burden placed on healthcare providers.
ADHA Chief Executive Tim Kelsey praised the addition of pathology and diagnostic organizations to the My Health Record platform. In Australia, pathology laboratory is the term to describe what are called clinical laboratories in the United States.
“The largest diagnostic organizations in Australia have now agreed to share their test reports with Australian consumers,” Kelsey said in an ADHA news release. “We are working to deliver a My Health Record for all Australians next year, unless they choose not to have one. Health consumers will benefit from this significant commitment by the pathology industry and their software partners.”

Australian Digital Health Agency CEO Tim Kelsey says his agency in 2018 will be creating a universal electronic health record for all the country’s 24.8 million citizens, though patients will have the option to opt out of the My Health Record project. He called the “significant commitment” of pathology labs to the project a major step forward. (Photo copyright: ADHA.)
In May 2017, Sonic Healthcare, Australia’s largest pathology provider, became the first private pathology company to join the My Health Record initiative. That news was followed by agreements between the ADHA and pathology companies Primary Health Care, Australian Clinical Labs, and seven other software vendors and pathology laboratories, including:
The ADHA also finalized service agreements with additional software companies that will enable diagnostic imaging providers to link up to My Health Record by the end of 2018.
AMA Says My Health Record Lacks Functionality and Critical Features
In 2012, Australia announced the roll out of the Personally Controlled Electronic Health Record, the original initiative to create a citizen-controlled secure online summary of health information, which later was renamed My Health Record. According to The Australian, more than 5.3 million Australians are now using My Health Record, a 500% increase in the number of shared health summaries uploaded in 2016-2017 and a 200% rise in interoperability with private hospitals.
Royal College of Pathologists of Australasia President Bruce Latham, MBBS, welcomed the announcement of the increased functionality for My Health Record.
“The Australian pathology sector has been working in support of the national eHealth agenda for a number of years,” Latham stated in the ADHA news release. “Work is now progressing to connect both public and private labs to the My Health Record, and patients nationally will start to see their pathology reports in their My Health Record.”
Developers and program administrators of My Health Record predict it will generate savings of AU$123 million from:
- Reduction in adverse drug events;
- Fewer duplicated diagnostics tests; and,
- Cost savings by 2020-2021.
However, the AMA, Australia’s doctors’ advocacy group, outlined its concerns about My Health Record in a Pre-Budget Submission to the Australian federal government. While praising the project’s potential to “not only save money, but save lives,” the AMA argued the national repository of healthcare information needs improved features and functionality to meet its potential.
“… more work is required,” the AMA wrote. “The return on investment will hinge in the short term on ease of use for medical practitioners who upload the clinical data. Interoperability with the multiple software packages used across the medical profession and broader health sector must be seamless.
“Problems uploading specialists’ letters, poor search functionality, time-consuming adaptations to existing medical practitioner work practices, or inappropriate workarounds will erode clinical utility and deter doctor use—and, more importantly, take time away from focusing on the patient,” the AMA concluded.
Automatic Enrollment Concerns AMA
My Health Record began as a self-register model, but as the program goes nationwide in 2018, it will do so using an “opt-out” model. This means citizens will be enrolled automatically unless they ask to be removed from the program. According to the ADHA, the automatic creation of My Health Record for all Australians will begin in mid-2018. The government’s goal is to provide access to My Health Record to all 24.6 million Australians by June 30, 2018.
The federal government’s switch to an opt-out system for My Health Record drew concerns from the AMA.
“Doctors do not have time to talk their patients through the My Health Record arrangements for opt-out, privacy, [or] setting access controls in standing consent for health providers to upload health information. This is the work of the government. Doctors must be allowed to focus on what they do best—caring for patients,” the AMA stressed.
Clinical Laboratories Have Stake in Outcome
According to Healthcare IT News Australia, the Australian government has spent AU$2 billion ($1.53 billion USD) so far developing what could become a white elephant if general practitioners and hospital groups don’t see a clinical benefit in its use.
If Australia is successful in creating a fully-functioning and widely-used national repository for health information, it will be among the first countries to do so. In 2002, the United Kingdom (UK) kicked off a nearly decade-long effort to create a national EHR system for the UK’s single-payer tax-supported health system. Ultimately, the government pulled the plug on the initiative after spending 12.7 billion pounds ($17 billion USD) trying to complete the project.
That result, and lessons learned from Australia’s experience, should inform American healthcare policy makers. It remains a daunting effort to implement a single electronic patient health records system. Of course, pathologists and clinical laboratory administrators have an interest in this issue, since medical laboratory test data represents the largest proportion of an individual patient’s permanent health record.
—Andrea Downing Peck
Related Information:
Australia’s Largest Pathology Labs Sign Up to My Health Record
Private Pathology Reports to Go Live in My Health Record
E-health Revolution Gather Pace as more Services Pledge their Backing
Australian Medical Association Pre-Budget Submission 2018-19
National Expansion of My Health Record in 2018 Confirmed in Budget Announcement
GPS and Hospitals Claim My Health Record Not Fit for Purpose as Alarming Low Usage Figures Are Released
Feb 7, 2018 | Digital Pathology, Laboratory Management and Operations, Laboratory News, Laboratory Operations, Laboratory Pathology, Laboratory Testing, Management & Operations
Federal agency receives input on eight focus areas as it looks for ways to enable providers ‘to design and offer new approaches to delivering care’
Medical laboratories and anatomic pathology groups preparing for the transition from fee-for-service healthcare will want to keep a close eye on the Centers for Medicare and Medicaid Services (CMS). The federal agency’s administrator plans to set a “new direction” for CMS as it shifts to value-based reimbursement models for Medicare services that could impact clinical laboratory revenues.
In an informal Request for Information (RFI), the Center for Medicare and Medicaid Innovation (CMMI) sought feedback on a “new direction to promote patient-centered care and test market-driven reforms that empower beneficiaries as consumers, provide price transparency, increase choices and competition to drive quality, reduce costs, and improve outcomes.”
CMS to ‘Move Away’ from Engineering Healthcare ‘From Afar’
The agency requested input on eight focus areas:
1. Increased participation in Advanced Alternative Payment Models (APMs);
2. Consumer-directed care and market-based innovation models;
3. Physician specialty models;
4. Prescription drug models;
5. Medicare Advantage innovation models;
6. State-based and local innovation;
7. Mental and behavioral health models; and,
8. Program integrity.
Comments from healthcare providers, clinicians, states, payers, and stakeholders were accepted through November 20, 2017.
In a Wall Street Journal (WSJ) op-ed, CMS Administrator Seema Verma explained the agency’s process moving forward. “We will move away from the assumption that Washington can engineer a more efficient healthcare system from afar—that we should specify the processes healthcare providers are required to follow,” she wrote.

CMS Administrator Seema Verma (above) plans to lead the Center for Medicare and Medicaid Innovation “in a new direction” and may be signaling a willingness to give providers more flexibility with value-based care payment models for Medicare services. (Photo copyright: Healthcare Dive.)
The RFI states the new model design will follow six guiding principles:
1. Choice and competition in the market;
2. Provider choice and incentives;
3. Patient-centered care;
4. Benefit design and price transparency;
5. Transparent model design and evaluation; and,
6. Small scale testing.
Providers Need Freedom to Design New Approaches to Healthcare
Verma said CMS plans to review all Innovation Center models to determine “what is working and should continue, and what isn’t and shouldn’t.” She voiced concern that the complexity of some of the current models may have encouraged consolidation in the healthcare system, resulting in fewer choices for patients.
“We must shift away from a fee-for-service system that reimburses only on volume and move toward a system that holds providers accountable for outcomes and allows them to innovate,” Verma wrote in the WSJ op-ed. “Providers need the freedom to design and offer new approaches to delivering care. Our goal is to increase flexibility by providing more waivers from current requirements.”
Actual Progress of Value-based Healthcare ‘Herky-Jerky’
In its reporting on the recent CMS announcements, Healthcare DIVE suggested that the U.S. Department of Health and Human Services (HHS) “is looking to make some potentially major changes” in value-based payment models.
However, Neil Smiley, CEO of Loopback Analytics, which assists healthcare organizations with managing outcome-based care, believes the transition to value-based care may face stiffer headwinds under the new administration. He points to an August CMS proposal that canceled some mandatory bundled payment programs and scaled back others as an indication that healthcare transformation could be slowing.
“The pace at which CMS committed to rolling out value-based care is fundamentally different from the pace we’re currently seeing,” he told Health IT. “The progress toward value-based care, instead of this steady momentum they expected, is more of a herky-jerky fashion.”
Modify, Don’t Abandon Existing Payment Models, suggests HCTTF
The Health Care Transformation Task Force (HCTTF), a 42-member industry consortium, was among the stakeholders who responded to CMS’ RFI. In a 22-page letter, the task force reiterated its support for the healthcare system’s transformation to value-based payment and care delivery, while outlining areas for improvements. The group urged CMS to continue to develop new models while modifying, rather than abandoning, existing models that show promise and need time to achieve a lasting return.
“We would like CMS to continue support for promising models while balancing the current portfolio with new, innovative payment models,” Clare Wrobel, Director of Payment Reform Models at HCTTF, told Home Health Care News. “[But] it would be a mistake to discard current models that providers have already invested in and are showing real promise.”
Smiley, meanwhile, suggests clinical laboratory managers, pathologists, and other healthcare providers keep watch as healthcare transformation continues to evolve.
“The fee-for-service model, love it or hate it, is not dying. The organism has adapted,” he told Health IT. “For those that were aggressive early adopters of value-based care and really believed what they were hearing, and have gone fully after value-based care, some of them may feel a little exposed. If they go too hard too fast, they may suffer economically if they misjudge the pace at which this moves.”
—Andrea Downing Peck
Related Information:
Centers for Medicare and Medicaid Services: Innovation Center New Direction
Medicare and Medicaid Need Innovation
CMS Seeks ‘New Direction’ for Innovation Center
Comprehensive Care for Joint Replacement Payment Model
Task Force Calls on CMS to Encourage Alternative Payment Models
CMS Request for Information: Innovation Center New Direction
Task Force Urges CMS to Preserve Value Based Payment Models