Jan 26, 2018 | Instruments & Equipment, Laboratory Instruments & Laboratory Equipment, Laboratory Management and Operations, Laboratory News, Laboratory Operations, Laboratory Pathology, Laboratory Sales and Marketing, Laboratory Testing, Management & Operations
Lack of Medicare or third-party payer coverage for most genetic screening tests in healthy adults is not discouraging development of new gene testing products
With the global anatomic pathology genetic testing market poised to reach $9.8 billion by 2025, clinical laboratories continue to develop new genetic screening tests (rather than diagnostic tests) intended to help physicians identify patients who carry inherited genetic mutations that could put them or their future children at higher risk for chronic disease, such as cancer.
This is a bit of a gamble since (with some exceptions) Medicare and many health insurers typically will not pay for predictive and presymptomatic genetic tests and services used to detect an undiagnosed disease or disease predisposition.
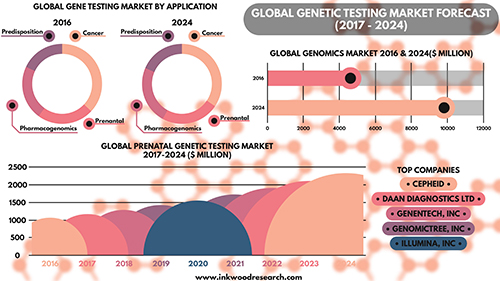
Nevertheless, Inkwood Research of Gurugram, India, predicts in its “Global Genetic Testing Market Forecast 2017-2024” report that aging populations throughout the world will be the driving force producing “enormous opportunities for the global genetic testing market.” The research firm anticipates this will result in a 9.93% increase in annual sales revenue during each of the next seven years.
Screening versus Diagnostic Testing Gains Popularity Among Patients, Physicians
Genetic diagnostic testing promises to accelerate the growth of precision medicine by guiding the diagnosis and treatment of cancer and other chronic diseases. However, genetic tests that “screen” healthy patients for predispositions to certain diseases also are gaining traction in the marketplace.
The US Food and Drug Administration (FDA) gave direct-to-consumer genetic screening testing a boost in April 2017 when it allowed marketing of 23andMe Personal Genome Service Genetic Health Risk tests for 10 inherited diseases or conditions, including:
· Parkinson’s Disease;
· Late-onset Alzheimer’s Disease;
· Celiac Disease; and
· other conditions.
“Consumers can now have direct access to certain genetic risk information,” Jeffrey Shuren, MD, Director of the FDA’s Center for Devices and Radiological Health, said in a press release. “But it is important that people understand that genetic risk is just one piece of the bigger puzzle, it does not mean they will or won’t ultimately develop a disease.”
Robert Green, MD, MPH, a Professor of Medicine at Harvard Medical School, told NPR that consumers should have access to genetic information. However, they also need to understand its limitations.
“Some people really want this [genetic] information on their own, and others want it through their physician,” Green said. “Both those channels are legitimate. People should just be aware that this information is complicated.”
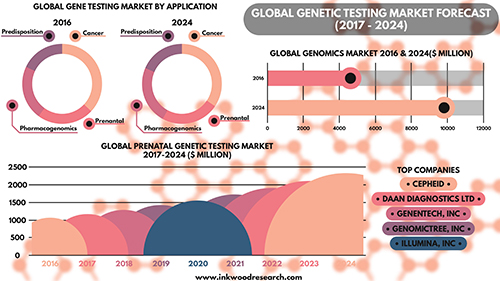
According to the Inkwood Research report, “The global genetic testing market is anticipated to grow from $4,614 million in 2016 to $9,806 million by 2025, at a CAGR [Compound Annual Growth Rate] of 9.93% between 2017 and 2025. The important driver increasing growth in the global genetic testing market is an aging population on the rise. The rising geriatric population is driving the global genetic testing market to a significant level.” (Caption and graphic copyright: Inkwood Research.)
· Cystic Fibrosis;
· Sickle Cell Disease; and
· Spinal Muscular Atrophy.
The genetic screening panel tests for the 22 heritable diseases cited by the American College of Obstetricians and Gynecologists (ACOG) in a Committee Opinion on genetic carrier screenings published by the ACOG in March 2017.
“The United States is truly a melting pot, and it no longer makes sense for physicians to assume genetic screening is appropriate for an individual based on presumed race or ethnicity,” Felicitas Lacbawan, MD, Executive Medical Director, Advanced Diagnostics, Quest Diagnostics, stated in a press release. “QHerit is designed for any woman and her partner, not just those in a specific, so-called high-risk ethnic or racial group.”
Genetic Screening in Primary Care Helps Assess Risk for Chronic Disease
Genetic diagnostic test developer Invitae (NYSE:NVTA) also points to growing evidence of the genetic screening test’s value to healthy individuals. In September 2017, Invitae presented initial findings at the National Society of Genetic Counselors 36th Annual Conference. The study showed a retrospective analysis of 120 patients tested with a proactive genetic screening panel for healthy adults had revealed medically significant findings for nearly one in five patients.
“Interest among otherwise healthy adults in using genetic information to understand their risk of disease conditions continues to grow each year, ” Robert Nussbaum, MD, Chief Medical Officer of Invitae, said in a press release. “These and other data show that interest is well-placed, with a substantial group of patients showing genetic variants associated with elevated risk of diseases like cancer where monitoring and early intervention can be helpful. Use of genetic screening in the primary care setting can assess risk to help shape individual screening plans. We are continually adding tools and resources that help reduce barriers to the widespread use of genetic information in mainstream medical practice.”
Routine Genetic Screening Could Become Norm, CDC Says
The Centers for Disease Control and Prevention (CDC) notes that newborn screening is “currently the largest public health genetics program in the world,” with more than four million babies screened at birth each year for 30 or more genetic conditions. In the CDC’s “Genomics and Health Impact Blog,” the agency continues to maintain a “cautionary attitude about personal genomic tests” beyond the newborn period, directing those considering direct-to-consumer laboratory testing, such as 23andMe and MyMedLab, to “think before you spit.”
Nonetheless, the CDC acknowledges routine genetic screening of healthy people could become the norm. However, others advise caution.
“To be sure, while the use of genome sequencing is promising in certain clinical scenarios, such as rare diseases and cancer, we do not think that whole genome sequencing in the general population is appropriate at this time,” Muin J. Khoury, PhD, MD, Director, Office of Public Health Genomics, CDC, wrote in a January 30, 2017, blog post. “We would not recommend its use outside research studies … But it is also becoming clearer that as science progresses, we are discovering more opportunities for using genetic screening of healthy individuals for preventing common diseases across the lifespan, outside of the newborn screening context.”
The impact on clinical laboratories and anatomic pathology groups should genetic screening become normalized should be clear: Labs will be tasked with performing these tests, and pathologists will be needed to interpret them and educate both physicians and patients on the findings.
Before that, however, genetic screening tests will need to be fully supported by government, and insurers, including Medicare, will have to agree to pay for them.
—Andrea Downing Peck
Related Information:
Global Genetic Testing Market Forecast 2017-2024
Carrier Screening for Genetic Conditions
Quest Diagnostics Launches QHerit, a Pan-Ethnic Genetic Screening Panel Aligned with New Medical Guidelines
Invitae Expands Test Menu for Proactive Genetic Testing in Healthy Adults
Invitae Highlighting New Research, Expanded Suite of Services at National Society of Genetic Counselors (NSGC) 36th Annual Conference
Consumer Genetic Testing: Think Before You Spit, 2017 Edition
Genetic Screening of Healthy Populations to Save Lives and Prevent Disease
FDA Allows Marketing of First Direct-to-Consumer Test that Provide Genetic Risk Information for Certain Conditions
FDA Approves Marketing of Consumer Genetic Tests for Some Conditions
Jan 19, 2018 | Instruments & Equipment, Laboratory Instruments & Laboratory Equipment, Laboratory Management and Operations, Laboratory News, Laboratory Operations, Laboratory Pathology, Laboratory Testing, Management & Operations
This may especially benefit cancer research and treatment thanks to MALDI’s ability to provide pathologists with a view of the whole-tissue micro-environment
Though it may be years before Matrix-Assisted Laser Desorption Ionization (MALDI) mass spectrometry finds use in clinical applications, recent developments show medical laboratories and anatomic pathologists how one type of technology is being rapidly adapted for use in diagnosing cancers.
Richard Drake, PhD, Director of the Medical University of South Carolina (MUSC) Proteomics Center, notes the importance of MALDI to cancer research. “In the clinic, there has to be something that will facilitate looking at all this data—tools that will let the pathologists look at it as well as the mass spec person,” Drake told GenomeWeb.
“It has been known for decades that glycosylation changes on the cell surface promotes cancer progression and the way the immune system sees a tumor or doesn’t see a tumor,” he explained. “That’s the advantage of MALDI imaging. You’re looking at the whole tissue micro-environment, and particularly for cancer it turns out to be important.”
Imaging Mass Spectrometry Applications for Anatomic Pathology
MALDI uses mass spectrometry imaging technology to enable high-molecular identification and an overall view of tissue. It differs from liquid chromatography-mass spectrometry (LC-MS), which is a chemical analysis technique.
An article by News-Medical describes in detail how MALDI technology works:
“MALDI imaging works through the utilization of a matrix, an acidic aromatic molecule that absorbs energy of the same wavelength produced by the irradiating laser. The matrix transfers the substance being examined to the gas state, thereby producing ionization in a three-step process:
1. “Thin sample sections on a metal slide are first covered with the matrix and the procedure for extracting molecules of interest from the tissue into the matrix begins. The matrix can be applied both manually and automatically.
2. “The laser irradiates the sample only in the matrix layer, meaning the underlying tissue remains intact.
3. “The released molecules are transferred to the gas state as the matrix absorbs the laser energy. Ions are formed due to the addition or removal of protons when in the gas state.
“The irons are required for further analysis via the mass spectrometer. The metal slide is placed into a MALDI mass spectrometer where the spatial distribution of the biological molecules is mapped. Within the mass spectrometer, the tissue specimen is raster scanned forming a mass spectrum for each spot measured. Image processing software is then required to import the data from the mass spectrometer to allow visualization of the image produced.”

The above schematic illustrates “the identification of bacteria and yeast by MALDI-TOF MS using the intact-cell method. Bacterial or fungal growth is isolated from plated culture media (or can be concentrated from broth culture by centrifugation in specific cases) and applied directly onto the MALDI test plate. Samples are then overlaid with matrix and dried. The plate is subsequently loaded into the MALDI-TOF MS instrument and analyzed by software associated with the respective system, allowing rapid identification of the organism.” (Caption and image copyright: Clinical Microbiology Reviews/American Society for Microbiology.)
MALDI in Clinical Laboratories
MALDI experts at MUSC worked with researchers at Bruker Corporation, a developer of scientific instruments and analytical diagnostic solutions for cell biology, preclinical imaging, clinical phenomics and proteomics research, clinical microbiology, and for molecular pathology research. Bruker is reportedly working with labs in Europe on MALDI-based assays for clinical use.
Developing MALDI applications for use in clinical laboratories and anatomic pathology groups could result in major improvements. Imaging mass spectrometry could:
- make more molecular information available;
- reduce pathology’s subjectivity and intra-observer nature;
- enable more accuracy and ability to duplicate current pathology assays; and,
- pave the way for new assays to be made.
“MALDI-IMS [imaging mass spectrometry] identifies the distributions of proteins, peptides, small molecules, lipids, and drugs and their metabolites in tissues, with high spatial resolution. This unique capacity to directly analyze tissue samples without the need for lengthy sample preparation reduces technical variability and renders MALDI-IMS ideal for the identification of potential diagnostic and prognostic biomarkers and disease gradation,” noted authors of a MALDI study published in the July 2017 edition of Biochimica et Biophysica Acta Proteins and Proteomics.
“You can take a slide of tissue and essentially do metabolomics on it so that you can look at the intricate nature of what metabolism is happening within a tissue,” James MacRae, PhD, Head of Metabolomics at the Francis Crick Institute in London, told Technology Networks, which described development of new mass spectrometry imaging technologies as “potentially game-changing.”
Mass Spectrometry in Clinical Laboratories
This is just the latest in a string of scientific developments involving mass spectrometry over the past decade that are potential boons to clinical laboratories. In “Is Mass Spectrometry Ready to Challenge ELISA for Medical Laboratory Testing Applications?” Dark Daily reported on the development of a new technique from the Department of Energy’s Pacific Northwest National Laboratory that uses mass spectrometry to identify protein biomarkers associated with cancer and other diseases. Researchers dubbed the technique PRISM, which stands for Proteomics Research Information System and Management.
And in “Swiss Researchers Use New Mass Spectrometry Technique to Obtain Protein Data, Create Strategy That Could Lead to Clinical Laboratory Advances in Personalized Medicine,” Dark Daily reported on researchers at the Swiss Federal Institute of Technology in Lausanne and ETH Zurich who developed a new way to use mass spectrometry to explain why patients respond differently to specific therapies. The method potentially could become a useful tool for clinical laboratories that want to support the practice of precision medicine.
As mass spectrometry’s role in clinical laboratories continues to expand, MALDI technology development and research could eventually lead to tools and applications that enhance how anatomic pathologist view tissue specimens in the medical laboratory. Though the research is ongoing, the technology seems particularly suited to cancer research and treatment.
—Donna Marie Pocius
Related Information:
Technical Advances Position MALDI Imaging as Plausible Tool for Clinical Pathology
Bruker Introduces Novel Mass Spectrometry Solutions for MALDI Imaging, Metabolomics, Proteoform Profiling, and Toxicology at ASMS 2017
The Proteomics of Prostate Cancer Exosomes
MALDI Imaging
Matrix-Assisted Laser Desorption Ionization–Time of Flight Mass Spectrometry: A Fundamental Shift in the Routine Practice of Clinical Microbiology
Metabolomics and Health – On the Cusp of a Revolution
Is Mass Spectrometry Ready to Challenge ELISA for Medical Laboratory Testing Applications?
Swiss Researchers Use New Mass Spectrometry Technique to Obtain Protein Data, Create Strategy That Could Lead to Clinical Laboratory Advances in Personalized Medicine
Precision Medicine Summit Feb. 21, 2018
Jan 17, 2018 | Coding, Billing, and Collections, Instruments & Equipment, Laboratory Instruments & Laboratory Equipment, Laboratory Management and Operations, Laboratory News, Laboratory Pathology, Laboratory Testing, Management & Operations
Moving to market are the newest generation of LIMS products designed to serve clinical laboratories while supporting quality reporting initiatives and new sources of revenue
It was Bob Dylan who made a big hit out of the song, “The Times, They Are A-Changin’.” The same could be said for the next generation of software products designed for use by medical laboratories.
To be fully successful, these next-generation laboratory information management systems (LIMS) must be radically different than the generations that came before. For example, medical laboratories are frustrated with the many limitations of older LIS products that still incorporate software technologies that date back to the 1980s and 1990s, such as MUMPS, which stands for Massachusetts General Hospital Utility Multi-Programming System.
But the newest LIMS products must do more than simply incorporate the latest technologies in software and cloud-based services. They must support all the ways that clinical laboratories and anatomic pathology groups generate increased revenue. More specifically, all medical laboratories will be generating vast quantities of molecular and genetic data. Therefore, an effective LIMS must be capable of capturing that data while also enabling the lab to perform certain healthcare big data analyses in support of the referring physicians and parent hospitals.
There also will be the need for medical laboratories to use their LIMS capabilities to support the data reporting requirements of Medicare and private health insurers. Payers increasingly want providers to report their quality monitoring, patient outcomes, and certain cost-of-care parameters. All these are functions that older LIS (laboratory information systems) products were not developed to provide.
Anatomic pathology group stakeholders and clinical laboratory managers understand the vital importance of their LIMS. Laboratory and healthcare workflows depend on the system’s:
- efficiency;
- scalability that supports the growth of the lab and medical practice; and,
- flexibility to interface with modern, point-of-care telehealth technologies in ways that enable labs and practices to engage in today’s precision medicine healthcare initiatives.
The more immediate need is for a LIMS to be capable of supporting Medicare’s Quality Payment Programs (QPPs), primarily the MACRA Merit-based Incentive Payments System (MIPS). Most physicians, including pathologists, will participate in MIPS. The first Medicare incentives or penalties will be paid next year, based on 2018 metrics and performance.
Given all these changing demands of advanced software technologies and the need for medical laboratories to participate in various value-based revenue programs, how might a LIMS empower labs to ensure success and increased revenue?
Quality Payment Programs and Merit-based Incentives
As part of the shift toward value-based care, the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) works to drive down costs and increase quality within both care and laboratory environments. MACRA establishes a data-driven payment system to reimburse service providers based on the outcome of services and care episodes, instead of the volume of services delivered or billed.
Combined with reduced payments, MACRA’s incentives and penalties, and Medicare’s QPP/MIPS payment programs, pressure has been increased on healthcare providers and medical laboratories alike. Thus, technology that gives labs a competitive edge is essential for thriving in an ever-evolving and increasingly competitive marketplace.
Meeting MACRA Goals with a Laboratory Information Management System
While electronic health record (EHR) systems have helped to consolidate patient protected health information (PHI), they do little to address the real-time creation of laboratory data and the accessibility of the massive volume of lab-related data stored in the average patient’s medical files.
A LIMS, however, helps to consolidate all this data in an easily accessible and powerful system. Some LIMS even combine with telehealth technologies to make data actionable and available at the point-of-care.
In this type of LIMS, laboratories, physicians, and other care providers all access the same dataset to ensure information is relayed quickly and efficiently. Interaction takes place using cloud-based interfaces, such as mobile apps or web portals. This ensures access to patient data and laboratory test results in a variety of locations without dependence on proprietary communications systems or hardware.
From bustling ERs and surgical wards to phlebotomists visiting long-term care facilities and mobile clinics, collecting and retrieving data becomes streamlined and accessible virtually anywhere.
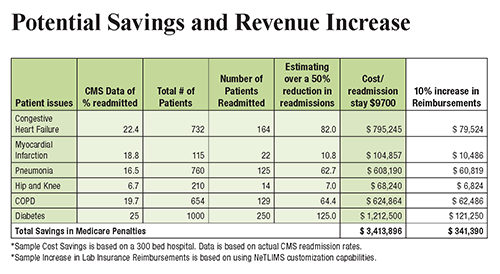
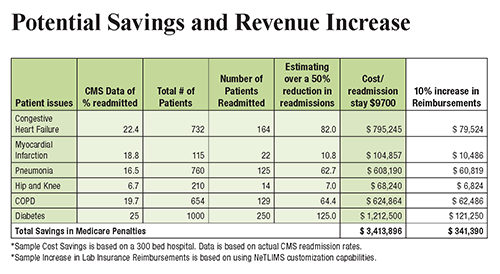
The chart above illustrates how a LIMS offers increased potential to automate processes and scale operations while keeping physicians, patients, and other critical parties up to date. This increase in efficiency and access to data empowers providers to reach improved patient outcomes and reduce hospital readmission rates, increasing revenue for both clinicians and clinical laboratories. (Graphic copyright: NetLIMS.)
When implemented properly, a LIMS also helps laboratories and healthcare facilities meet the terms of MIPS. This reduces Medicare penalties and ensures payment adjustments, which improve revenue streams even further.
Understanding LIMS and Cloud-Based Lab Systems
To help outline and explain the benefits of a LIMS for laboratories and healthcare facilities, The Dark Report, in conjunction with NetLIMS, a global provider of laboratory information management systems to hundreds of hospitals and commercial laboratories worldwide, has produced a free white paper titled, “The Path to More Revenue: Cloud-Based LIMS, Mobile Apps, and Point-of-Care Telehealth.”
- This white paper addresses critical concerns, including:
- Overviews of new technologies;
- The impact of value-based programs on the lab market;
- The importance of MACRA and MIPS adherence;
- How technology, such as a LIMS, can help labs achieve improved efficiency; and,
- Tips on choosing a LIMS vendor to maximize ROI.
To download your free copy of the whitepaper click on this link: Or, copy this URL into your browser: https://www.darkdaily.com/whitepaper/the-path-to-more-revenue-cloud-based-lims-mobile-apps-and-point-of-care-telehealth .
Thanks to advances in LIMS design and development, remote patient digital therapeutics, and cloud-based technology, healthcare providers now have unprecedented opportunities to better manage the health of patients with chronic conditions. In addition, it can help you achieve better efficiency, economics, and compliance with MACRA.
This free white paper is your first step toward significantly reducing hospital readmission rates, bridging the gap between labs, physicians, and other healthcare providers they serve, and positively affecting patient outcomes, improving quality measures, and maximizing reimbursements for all services you provide.
—Jon Stone
Related Information:
The Path to More Revenue: Cloud-Based LIMS, Mobile Apps, and Point-of-Care Telehealth
How Close Is the End of Private Practice Pathology as We’ve Known It?
Attention Anatomic Pathologists: Do You Know Medicare Is Prepared to Change How You Are Paid, Beginning on January 1, 2017?
Innovator Hospitals Bring ICUs into the Info Age, Using New Design Approaches that involve Medical Laboratory Tests
Jan 15, 2018 | Instruments & Equipment, Laboratory Instruments & Laboratory Equipment, Laboratory Management and Operations, Laboratory News, Laboratory Operations, Laboratory Pathology, Laboratory Testing, Management & Operations
Lab-on-skin is the latest concept to join the lab-on-a-chip, lab-in-a-needle, and lab-on-paper field, as researchers continue to seek ways to miniaturize medical laboratory tests
Move over, lab-on-a-chip and lab-on-paper. There’s a new diagnostic technology in research labs that is gaining credibility. It is called lab-on-skin technology and some scientists are quite excited about how it might be used for a variety of clinical purposes.
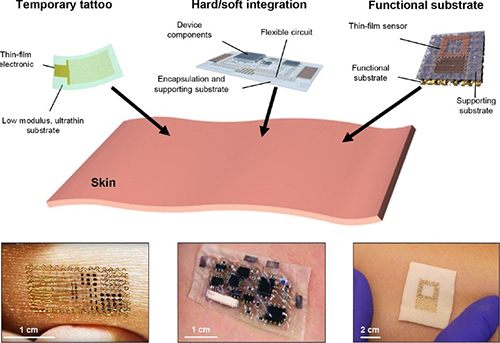
A recent story published in ACS Nano titled, “Lab-on-Skin: A Review of Flexible and Stretchable Electronics for Wearable Health Monitoring,” reviews the latest advancements in lab-on-skin technology. It provides an overview of different research initiatives incorporating lab-on-skin technologies.
From telehealth to precision medicine to point-of-care mobile devices, anatomic pathologist and clinical laboratories are about to be challenged with new diagnostic technologies. These technologies are intended to streamline the workflow between physicians and medical laboratories while improving access to patient data and medical laboratory test results.
Of all the mobile devices designed to support medical care, no technology may have more potential to change the pathology profession than nanotechnology-based diagnostic devices. Whether lab-on-a-chip, lab-in-a-needle, or lab-on-paper, these miniature laboratories are so small dozens can be carried in a pocket.
Most importantly, for certain diagnostic tests, some of these devices being developed hope to deliver full-size-lab quality results accurately and inexpensively, even in rural regions and areas with little or no resources, such as electricity or water. (See Dark Daily, “Lab-on-a-Chip Diagnostics: When Will Clinical Laboratories See the Revolution?” September 9, 2016.)
Now, researchers have demonstrated that even biomarkers within human skin can be tested by medical wearable devices. “Lab-on-skin” has entered the pathology vernacular.
Lab-on-Skin Constantly Measures Physiological Data
According to ACS Nano, lab-on-skin devices are small electronic patches worn directly on the skin that noninvasively measure a variety of physiological data. These flexible gadgets can interpret information including:
- body temperature;
- blood oxygenation;
- hydration;
- blood pressure;
- glucose;
- potassium;
- sodium; and,
- lactate and pH levels in individuals.
The devices may also be used for wound care, prosthetics and rehabilitation, as well as for optogenetics and human-machine interfaces (HMI).
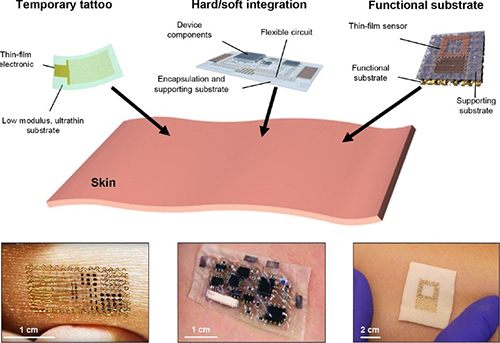
The image above from the ACS Nano article demonstrates various lab-on-skin devices, including: an NFC tattoo with a bare die chip mounted on an acrylic adhesive film; a soft radio sensor with commercial chips encapsulated in a fluid/ecoflex package; and, a sweat sensor on silicone foam. Each of these devices could be capable of delivering actionable diagnostic data to anatomic pathologists and clinical laboratories. (Image copyright: ACS Nano.)
Lab-on-skin technology can be utilized to read electrophysiological signals typically measured by electrodes placed on various parts of the body, such as:
The direct connection between the patches and the skin allows for continuous and precise data collection without the threat of drying out that comes with traditional electrodes.
Nanotechnology Driving Clinical Laboratory Diagnostic Applications
Because it is the largest organ in the body, skin provides a perfect pathway to convey biological information originating from various parts of the body, such as inner organs, muscles, blood vessels, and the dermis and epidermis.
The ACS Nano article discusses advancements in the designs and materials used for lab-on-skin patches. In addition to the term “lab-on-skin,” these devices may also be referred to as electronic skin, epidermal electronics, and electronic tattoos. They have untapped potential in a variety of clinical applications, including:
For example, researchers at the University of Illinois at Urbana-Champaign have created an epidermal nanotechnology device that utilizes sensors and wireless interfaces to measure ultraviolet (UV) exposure, a risk factor for skin cancers.
“Our goal with this research is to establish a set of foundational materials and device designs for systems that can improve health outcomes by providing information on UV exposure,” John A. Rogers, PhD, and Professor of Materials Science and Engineering and Professor of Chemistry told Nanowerk Spotlight.
Nanotechnology employs extremely small particles performed at the nanoscale (about 1 to 100 nanometers). This field is emerging as a vital element behind cutting-edge innovations in medicine and healthcare.
“We developed new chemistries that yield color changes that quantitatively relate to total exposure dose, separately in both the UV-A and UV-B regions of the solar spectrum,” explained Rogers. “Our formulations have the additional advantage that they provide soft, low modulus mechanics to enhance comfort and biocompatibility with the skin surface.”
Mini-Laboratory Devices Could Push Pathology Data to Clinical Laboratories
The combination of using lab-on-skin devices with nanotechnology can provide researchers and medical professionals a multifunctional and valuable tool for health monitoring and the diagnosis of diseases. However, more research and clinical studies are needed to establish the validity of using lab-on-skin devices in healthcare applications.
Nevertheless, clinical laboratories and pathology groups will be handling more data in the future, generated by these miniature laboratory devices. Their usefulness, especially in challenging healthcare environments, is only beginning to be fully discovered.
—JP Schlingman
Related Information:
A Lab-on-Skin: A Review of Flexible and Stretchable Electronics for Wearable Health Monitoring (downloadable PDF)
Lab-on-Skin: A Review of Flexible and Stretchable Electronics for Wearable Health Monitoring (original ACS Nano article)
Lab-on-Skin: Nanotechnology Electronics for Wearable Health Monitoring
Stick-on Epidermal Electronics Tattoo to Measure UV Exposure
Nanotechnology in Healthcare (Part 1: Fitness Monitoring, Diagnostics and Prevention)
Nanotechnology in Healthcare (Part 2: Nanomedicine Therapy)
Breathable, Wearable Electronics on Skin for Long-term Health Monitoring
Nano-chip Promises to Heal Organs at a Touch
IBM and Mount Sinai Researchers Develop Innovative Medical Lab-on-a-Chip Solution
Lab-on-a-Chip Diagnostics: When Will Clinical Laboratories See the Revolution?
Researchers at University of Rhode Island Unveil Lab-on-Paper Test Capable of Multireagent Diagnostics: Could Enable ‘Diagnostics Without the Lab’ Say Developers
Sleek ‘Lab in a Needle’ Is an All-in-One Device That Detects Liver Toxicity in Minutes during a Study, Showing Potential to Supplant Some Medical Laboratory Tests
Jan 10, 2018 | Compliance, Legal, and Malpractice, Instruments & Equipment, Laboratory Instruments & Laboratory Equipment, Laboratory News, Laboratory Pathology, Laboratory Testing
CMS sends letter to Orig3n notifying the genetic test company that it may not have the required certifications to market its genetic tests
Orig3n’s recent ill-fated “DNA Day” promotion to offer free genetic tests during an NFL football game this past fall pushed Orig3n into the media spotlight. The Massachusetts-based biotech company—which sells 18 different DNA tests on its website—suspended the promotion due to questions from the Centers for Medicare and Medicaid Services (CMS) and the Maryland Department of Health (MDH) regarding the legality of the testing under the Clinical Laboratory Improvement Amendments of 1988 (CLIA).
Since then, however, new details from BuzzFeed and GenomeWeb indicate that Orig3n may not have the required certifications to market their genetic tests after all. On October 30, 2017, CMS served Orig3n with an out-of-compliance notice. According to BuzzFeed, the letter came from Karen Dyer, MT (ASCP) DLM, Director, Division of Laboratory Services and the CLIA program at CMS.
In a letter to Kate Blanchard, Chief Operating Officer at Orig3n, Dyer wrote, “To apply for CLIA certification, Orig3n must contact both the Massachusetts and California state agencies immediately for guidance. Orig3n’s various tests analyze 18 genes related to health, from ‘muscle power’ to ‘sugar sensitivity’ to ‘age-related metabolism’. It offers genetic testing that provides information for the assessment of health.” The letter gave Orig3n a November 13 deadline to update CMS on issues regarding their CLIA certification.
Robin Smith, CEO, Orig3n, told GenomeWeb the notice “was the first time that any clear guidance was given regarding specific genes and requirements for CLIA/non-CLIA.” He also noted efforts Orig3n undertook over the prior year to fully certify their laboratory.

The test shown above is one of 18 genetic tests Orig3n offers direct to consumers. According to Vice, Orig3n claims their tests do not require FDA-approval “because the tests are not diagnostic [and] they don’t require it.” The Baltimore Sun reported that “Orig3n is confident it can receive the proper approvals and plans to have a fan giveaway later this season at one of our games.” (Photo copyright: Orig3n.)
Fortunately for Orig3n, meeting compliance and obtaining certification for their existing lab is no longer a requirement to resolve the issue. In a November press release, Orig3n announced the purchase of Interleukin Genetics. Orig3n plans to absorb Interleukin’s existing assets, including a CLIA-certified genetics laboratory in Waltham, Mass., capable of analyzing more than one million samples annually.
“Once we met with Interleukin Genetics, we saw a natural alignment between the two organizations regarding our shared commitment to a future of personalized health,” Smith noted. “With our trajectory of accelerated growth, we couldn’t imagine a better fit for acquisition. We are very pleased to be welcoming Interleukin Genetics to Orig3n.”
GenomeWeb asked Blanchard how the acquisition would impact Orig3n’s commercialization of the 18 tests in question by CMS, now that Orig3n owns a CLIA-certified lab, and through it, meets the requirements of CMS’ out-of-compliance notice. Blanchard declined to comment.
New Concerns Surrounding Interleukin Assets
Yet, in solving one set of problems, some experts believe Orig3n might have inherited a new set. In July 2016, GenomeWeb reported that Interleukin Genetics would be laying off 63% of its staff. Unable to secure a clinical services agreement, the company could not extend debt payment deferrals with its senior lenders. At the time of writing, debts totaled $5.6 million.
Further complicating matters, a 2015 peer-reviewed analysis published in the Journal of the American Dental Association (JADA) questioned the clinical validity of an inflammation management program called “Ilustra” that Interleukin claimed, “identifies individuals with an increased risk for severe and progressive periodontitis, due to a life-long genetic predisposition to over-produce Interleukin-1 (IL-1), a key mediator of inflammation.”
Another GenomeWeb article reported on the turbulent road the Ilustra program followed until Orig3n eventually pulled it from the market. GenomeWeb noted critics’ concerns about the marketing of precision medicine, genetic testing, and regulatory issues facing medical laboratories as these technologies mature.
Clinical Laboratories Continue to Field Concerns Over DTC Testing
“This [genetic] test would have been laughed out of the room if it had been presented to oncologists, or to professionals in medical genetics,” declared Scott Diehl, PhD, co-author of the JAMA analysis, a genetics researcher at Rutgers School of Dental Medicine, and Professor and Principal Investigator at Rutgers Biomedical Health Sciences.
GenomeWeb notes in their latest coverage that with Orig3n’s purchase of Interleukin Genetics, Diehl is once again concerned that the genetic tests in question might find their way back to the market.
When GenomeWeb questioned Orig3n about the concerns surrounding Interleukin’s Ilustra product, a spokesperson stated, “that was simply before Orig3n’s time with the company and they do not have a part in it.” Blanchard added, “[We are] looking at the entire Interleukin portfolio and implementing the tests if and when we decide it is appropriate.”
Regardless of the decisions made by Orig3n on future genetic tests and genetic service offerings, coverage of this event highlights a myriad of concerns—from regulatory scrutiny to the pitfalls of acquiring existing diagnostic tests or laboratory assets—facing clinical laboratories, anatomic pathologists, and other medical professionals working in the ever-shifting landscape of the modern healthcare system.
—Jon Stone
Related Information:
This DNA Testing Company Is Violating Federal Lab Testing Rule
Orig3n Acquires Interleukin Genetics, a Genetics-based Personalized Health Company, to Advance the Future of Health Faster
Orig3n’s Purchase of Interleukin’s CLIA Lab May Appease CMS, But Some Question Plans for Test Assets
Biotech Company Offers Fitness and Beauty-Focused Genetic Tests
Interleukin Genetics Slashes 63 Percent of Workforce, Shuts down Program and Mulls Sale
‘DNA Day’ Planned for Ravens Game Undergoes Federal and State Scrutiny
Interleukin Shutting Down Genetic Testing Program, Lays Off Staff
Divergent Findings on Interleukin Gum Disease Risk Test Raise Questions about Clinical Use
Interleukin 1 Genetic Tests Provide No Support for Reduction of Preventive Dental Care
Controversial Gum Disease Risk Test Highlights Precision Medicine Marketing, Regulatory Issues
State and Federal Agencies Throw Yellow Flag Delaying Free Genetic Tests at NFL Games in Baltimore—Are Clinical Laboratories on Notice about Free Testing?
Jan 8, 2018 | Instruments & Equipment, Laboratory Instruments & Laboratory Equipment, Laboratory Management and Operations, Laboratory News, Laboratory Pathology, Laboratory Testing
Microbiome is once again leading scientists toward a new understanding of how human gut bacteria can impact the efficacy and side-effects of certain cancer therapies
Anatomic pathology researchers already know that a person’s genetics can affect the results of cancer treatments. Now it is becoming clear that a patient’s microbiome—which includes gut bacteria—may also impact the efficacy of particular cancer treatments. A recent study showed that gut bacteria can be used to determine whether a cancer drug will work for a certain individual and also if the patient might suffer side effects from certain cancer treatments.
Working with this knowledge, diagnostic test companies may possibly develop new clinical laboratory tests designed to help physicians better diagnose and treat cancer patients. This, in turn, advances personalized medicine and treatments for chronic diseases tailored to patients’ specific physiologies and conditions. This is a healthcare trend where medical laboratories can expect to play a critical role.
Gut Bacteria as Important as Genetics in Cancer Treatments
A recent article published in the journal Nature: npj Biofilms and Microbiomes, outlined a correlation between gut bacteria and side effects of irinotecan (sold as Camptosar), a drug used to treat metastatic colorectal cancer.
Libusha Kelly, PhD, Assistant Professor in the Departments of Systems and Computational Biology, and Microbiology and Immunology, led researchers from the Albert Einstein College of Medicine located in Bronx, N.Y., in conducting the study.
“We’ve known for some time that people’s genetic makeup can affect how they respond to a medication,” noted Kelly in an Einstein news release. “Now, it’s becoming clear that variations in one’s gut microbiome—the population of bacteria and other microbes that live in the digestive tract—can also influence the effects of treatment.”
Irinotecan is administered intravenously to colorectal cancer patients in an inactive form and is metabolized to an active form by liver enzymes. The drug is later converted back to an inactive form by other liver enzymes and the addition of a Glucuronidase chemical group. The irinotecan then enters the intestine for expulsion by the body.

Taken from the Einstein College of Medicine published study, the graph above illustrates “Two distinct metabolizer phenotypes or ‘metabotypes’ based on % SN-38 formation during a time course incubation of SN-38G with fecal samples from 20 individuals quantified by LC-MS/MS. Participants were sub-grouped into low (n = 16) and high (n = 4) metabolizer phenotypes. All samples were run in triplicate and values are the mean ± sem.” (Graphic copyright: Nature/Albert Einstein College of Medicine.)
However, bacteria residing in the digestive tract of some individuals prevent the medication from metabolizing properly and reactivates the medication, which transforms the irinotecan into a toxic substance that can cause side effects.
To perform the research, Kelly and her team collected fecal samples from 20 healthy individuals and treated those samples with inactive irinotecan. The samples were then examined and categorized by whether or not they were able to metabolize or reactivate the drug.
Identifying Potential for Side Effects in Patients a Powerful Tool for Medical Laboratories
Irinotecan can cause severe diarrhea and dehydration in up to 40% of patients who take the medication. By focusing on the presence of beta-glucuronidase (enzymes that are used to catalyze the breakdown of complex carbohydrates) the researchers found that gut bacteria can also be used to distinguish which patients will encounter side effects from the drug.
“As you can imagine, such patients are already quite ill, so giving them a treatment that causes intestinal problems can be very dangerous,” said Kelly in the news release. “At the same time, irinotecan is an important weapon against this type of cancer.”
Four of the 20 subjects in the study were determined to be high metabolizers. Due to differences in the composition of their microbiomes, the team concluded that the high metabolizers were more likely to experience side effects from irinotecan.
The research also demonstrated that beta-glucuronidase enzymes in the gut may adversely interact with some commonplace drugs, such as ibuprofen and other nonsteroidal anti-inflammatory medications (NSAIDs), morphine, and Tamoxifen, a drug that is prescribed mainly to breast cancer patients.
“In these cases, the issue for patients may not be diarrhea,” states Kelly in the news release. “Instead, if gut bacteria reactivate those drugs, then patients might be exposed to higher-than-intended doses. Our study provides a broad framework for understanding such drug-microbiome interactions.”
Microbiome Takes Center Stage in Pathology Research
As Dark Daily previously reported, from extending life to developing more powerful treatments for chronic diseases, the human microbiome is quickly becoming an important subject of research studies. The findings from such studies will trigger advances in precision medicine. And, the clinical laboratory assays developed from this research will give physicians the knowledge needed to select the most appropriate drug therapies and treatments for individual patients.
—JP Schlingman
Related Information:
Gut Bacteria Can Stop Cancer Drugs from Working
Gut Microbiome May Make Chemo Drug Toxic to Patients
Human Microbiome Signatures of Differential Colorectal Cancer Drug Metabolism
Researchers in Two Separate Studies Discover Gut Microbiome Can Affect Efficacy of Certain Cancer Drugs; Will Findings Lead to a New Clinical Laboratory Test?
Attention Microbiologists and Medical Laboratory Scientists: New Research Suggests an Organism’s Microbiome Might Be a Factor in Longer, More Active Lives
Mayo Clinic and Whole Biome Announce Collaboration to Research the Role of the Human Microbiome in Women’s Diseases Using Unique Medical Laboratory Tests