May 30, 2018 | Laboratory Hiring & Human Resources, Laboratory Management and Operations, Laboratory News, Laboratory Operations, Laboratory Pathology, Laboratory Sales and Marketing, Laboratory Testing, Management & Operations
As healthcare continues to expand outside of traditional environments, clinical laboratories must adapt to providers’ changing needs
Healthcare settings continue to pop up in non-traditional locations. For years, clinical laboratories and anatomic pathology groups have had to adopt to a changing healthcare landscape, such as the trend to move care out of hospitals and doctor’s offices to lower costs and improve access.
In some instances, treating patients in their homes is safer for patients’ health. (See Dark Daily, “Hospital-in-the-Home Shows Promise for Reducing Acute Care Costs; Medical Laboratories Face Uncertainties Concerning Expanding Services to In-Home Environments in Support of Care Providers,” May 2, 2018.) Similarly, receiving care at retail locations such as Rapid Clinics—including clinical laboratory procedures and testing—offers many advantages for busy patients. Dark Daily has reported on these trends as far back as 2011. (See Dark Daily, “More Medical Laboratory Testing Expected as Retail Clinics Change Delivery of Routine Healthcare Services,” October 24, 2011.)
It’s a win-win for healthcare organizations and patients alike that shows no sign of slowing down. Thus, it should come as no shock that retail giant Walmart (NYSE:WMT) would want to remain competitive in this high-value consumer market.
Walmart Continues Expansion into Healthcare Market
Walmart Care Clinics, which are primarily staffed by certified nurse practitioners, are currently operating in Georgia, South Carolina, and Texas, according to Healthcare Finance. Caregivers in those clinics are trained to diagnose and treat a wide variety of basic medical conditions, including:
- Managing chronic conditions;
- Performing lab tests;
- Administering vaccinations;
- Making referrals; and,
- Prescribing medications.
Now, possibly in a bid to compete with CVS and Walgreens, Walmart has announced plans to allocate part of an $11-billion remodeling project to include private consultation rooms in hundreds of its store pharmacies. These rooms will allow customers to have confidential discussions about their medications and healthcare with pharmacists and other pharmacy staff members.
The majority of the store renovations will occur in Florida and Texas where the company has allotted $477 million to remodel 82 stores and add 14 new stores.
Walmart Health App and Wellness Days
Another step Walmart is taking to compete in the healthcare space involves mobile software. In May, Walmart announced it was partnering with digital health company Sharecare to provide employees and community members with access to the Sharecare mobile healthcare app. The app enables users to complete personalized health profiles and track their health.

Walmart Wellness Days are a quarterly in-store event designed to educate community members on ways to make positive changes in their health. Might clinical laboratories one day be performing medical laboratory and pathology testing ordered by physicians and nurse practitioners located in retail Walmart pharmacies? (Photo copyright: Walmart.)
“Walmart is committed to helping our associates, their families, and communities to improve their overall wellbeing through wellness programs,” Jacqui Canney, Executive Vice President and Chief People Officer at Walmart, stated in a press release. “Partnering with Sharecare will provide our associates additional tools to inspire them on their wellness journey, help our programs continue to grow, and be a force for change in the communities we serve.”
Sharecare sees this relationship as both disruptive and transformative, not just for a company’s employees and customers, but for the entire nation.
“As we have learned from our research through the Gallup-Sharecare Well-Being Index, a person’s holistic wellbeing is defined by five essential elements—purpose, social, financial, community, and physical—and when those elements are in alignment, individuals and places exhibit greater adaptability to change, resiliency, and productivity in the workplace, among other benefits,” noted Dan Witters, Research Director for the Gallup-Sharecare Well-Being Index, in the press release. “As the nation’s single largest employer with more than 1.5 million associates, Walmart and Sharecare have the potential to disrupt the status quo of workplace wellness and transform the health not only of the communities in which Walmart operates, but also, ultimately, our country.”
Lofty expectations, to be sure. Nevertheless, for clinical laboratories to remain competitive, they must be prepared to adapt and serve healthcare providers in any location. Increasingly, these caregivers are finding themselves treating patients outside of traditional healthcare environments in locations convenient to healthcare consumers, such as retail environments.
—JP Schlingman
Related Information:
Walmart is Remodeling 500 Stores as Part of an $11 Billion Spending Plan—Here’s How Stores Will Change
Walmart Signals Continued Interest in Healthcare Space Through Remodel of Pharmacies
Walmart Partners with Sharecare to Transform the Health and Wellbeing of Their Associates and Communities
Hospital-in-the-Home Shows Promise for Reducing Acute Care Costs; Medical Laboratories Face Uncertainties Concerning Expanding Services to In-Home Environments in Support of Care Providers
More Medical Laboratory Testing Expected as Retail Clinics Change Delivery of Routine Healthcare Services
May 9, 2018 | Compliance, Legal, and Malpractice, Laboratory Hiring & Human Resources, Laboratory Management and Operations, Laboratory News, Laboratory Operations, Laboratory Pathology
Supreme Court of India ruling may finally ignite a crackdown on illegal medical laboratories that operate without a licensed pathologist
What would happen if 80% of Americans did not trust the medical laboratories that run their diagnostic tests? What impact would that have on this country’s clinical laboratory and anatomic pathology industry? Certainly, a significant one.
Well, that’s exactly what has happened in India. A survey on graft in India’s healthcare system conducted by LocalCircles, a community social media platform, has highlighted citizens’ distrust and disgust with the nation’s pathology laboratories. Only 20% of the 29,000 citizens surveyed said they “fully trusted” the pathology lab they use, while 32% of respondents said they had received one or more incorrect pathology reports in the past three years.
In India, the term “pathology laboratories” describes what are called clinical laboratories in the United States and Canada. Histopathology laboratories in India perform testing on tissue, just as anatomic pathology and surgical pathology laboratories do in North America.
According to the survey results, 91% of respondents believe clinical laboratories should lose their licenses if found to be giving incentives to doctors for prescribing tests. In addition:
- 86% of those surveyed feel doctors’ earnings in hospitals should be unrelated to the value of tests they refer to the hospital’s pathology lab; and,
- 59% believed kickbacks from labs incentivized doctors to prescribe unnecessary tests.
“One of the important cogs in the wheel of the medical system in our country are the pathology labs,” LocalCircles noted in the survey results. “Being a high profit business, thousands of them have mushroomed in different parts of the country. Many people say these pathology labs have a tie up with the doctors and pass on a commission to the doctors for every patient they send to them.”
India’s Medical Laboratories Under Increasing Scrutiny
The LocalCircles survey underscores the ongoing concerns in India over the quality of its medical laboratories, which have come under fire for lack of regulations and accreditation standards.
In India, the term “pathology” describes a laboratory performing standard medical laboratory tests, such as chemistry, hematology, immunoassay, and microbiology. Histopathology is the term used to describe diagnostic testing that utilizes tissue specimens.
Last year we reported on the tens of thousands of lab companies that continue to operate in India without certified pathologists and other trained lab scientists. (See Dark Daily, “Shortage of Registered Pathologists in India Continues to Put Patients at Risk in Illegal Labs that Defy Bombay Court Orders,” April 12, 2017.)
Technicians Cannot Run Pathology Laboratories, Supreme Court of India Rules
There are signs, however, that the tide may be turning against unqualified pathology labs. Last year, The Supreme Court of India upheld a lower court order that directed only a “qualified and registered pathologist, with a postgraduate qualification in pathology” can countersign a patient’s pathology report, the Times of India (TOI) reported.
The TOI quoted an unnamed senior food and drug department official as saying, “Many technicians with [a] diploma in Medical Laboratory Technology and other equivalent qualifications are operating pathology laboratories,” because no laws currently exist requiring a qualification in pathology as a prerequisite for running a private laboratory.
“If unqualified people certify medical reports, it will hamper patient treatment,” Sadhana Kothari, MD, Associate Professor, Department of Pathology at Gujarat Cancer Society Medical College in Gujarat, India, told the TOI. “A doctor’s analysis and patient’s treatment [are] dependent on clinical tests. The Supreme Court judgment will ensure that illegal labs do not operate.”
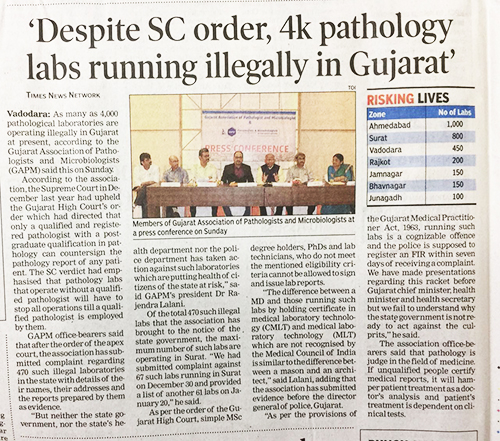
Local press coverage like that above highlights the severe pressure India’s pathology laboratory industry faces following the Supreme Court of India’s ruling that only qualified and registered pathologist—with a postgraduate qualification in pathology—can run pathology laboratories or sign off on pathology reports. (Image copyright: VAPM Pathologists and Microbiologists Welfare Society.)
Illegal Labs Continue to Operate Despite India Court Rulings
The Supreme Court decision means that PhDs, laboratory technicians, and others without proper medical credentials can no longer sign laboratory reports. The Supreme Court verdict emphasized that labs operating without a qualified pathologist should cease operations until a qualified pathologist can be hired. However, earlier verdicts in the Indian court system have failed to end the proliferation of illegal labs.
According to the TOI, the Association of Practicing Pathologists (India) (APPI) first filed a writ in 1998 to prevent individuals not qualified in pathology and/or registered with the Medical Council of India from running laboratories. In 2010, the Gujarat High Court ruled, “Laboratory technicians are not pathologists and cannot run any laboratory independently.”
A month after the Gujarat High Court decision, pathologists in Gujarat complained the state government had failed to initiate criminal action against people running unauthorized labs. The Indian Express reported the Gujarat Association of Pathologists and Microbiologists was starting a public awareness campaign to stop illegal labs from operating because the state government had not shut down illegal operators.
Number of Qualified Pathologists Decreasing
The ruling by the Supreme Court of India, however, may result in concrete action being taken by the states. On February 6, 2018, the Pune Mirror reported the Maharashtra State Human Rights Commission (MSHRC) ordered the state public health department and the director of medical education and research to identify and take action against labs working without valid licenses.
According to the Pune Mirror, only 2,200 of the state’s 10,000 diagnostic laboratories are headed by certified pathologists. The Maharashtra Association of Practicing Pathologists and Microbiologists (MAPPM), the largest body of certified pathologists in the state, claims as many as 8,000 pathology labs in Maharashtra function without licenses.
“The state government has the mechanism to keep a tab on such labs, but they don’t take action,” Sandeep Yadav, MD, President of MAPPM, told the Pune Mirror. “It has become an easy way to earn money because there is no law yet around registering labs. Many people open laboratories simply by observing pathologists over time, and it could be a threat to a patient’s life, as it has been observed that many labs are illegal or run by technicians. The number of qualified pathologists is decreasing and genuine people don’t want to pick up the profession.”
Also in February 2018, the New India Assurance Company, the country’s largest insurer, instructed its regional offices to not approve medical claims from pathology laboratories if the reports are signed by unlicensed and unqualified staff, the Pune Mirror reported.
The challenges of providing first-line medical laboratory testing services in countries like India demonstrate how expectations of quality and accuracy are driving change in these rapidly-developing nations. It is a reminder to clinical laboratory managers and pathologists in the United States that the trust of patients and government regulators is a valuable asset.
—Andrea Downing Peck
Related Information:
Majority Say a Corrupt Nexus Exists Between Pathology Labs and Doctors
GAPM: Bogus Pathology Labs Playing with People’s Lives
State to Crack Down on Illegal Path Labs
Pathologists Start Awareness Campaign after HC Order
Pathologist Body Launches Campaign Against Rogue Labs
Insurance Major Says No to Illegal Lab Reports
Shortage of Registered Pathologists in India Continues to Put Patients at Risk in Illegal Labs that Defy Bombay Court Orders
Apr 23, 2018 | Compliance, Legal, and Malpractice, Laboratory Hiring & Human Resources, Laboratory Instruments & Laboratory Equipment, Laboratory Management and Operations, Laboratory News, Laboratory Operations, Laboratory Pathology, Management & Operations
Critics are quick to note that this creates a disparity in how patients access healthcare services
Independent concierge care (AKA concierge medicine) is available to anyone willing to pay the additional costs, which are over and above any health insurance. In a concierge care medical practice, patients pay an annual retainer fee to gain increased access to doctors, specialists, and services, such as faster TATs on clinical laboratory testing.
Depending on the program, concierge care also can offer patients a range of “improved” healthcare benefits, including same-day appointments, extended appointment times, around-the-clock telehealth services, and the experience of receiving care from a physician with a smaller patient roster and in a more personalized manner.
Clinical laboratories and anatomic pathology groups might also find benefit from the concierge care model. Though some concierge providers bill insurance, most work on a cash basis with payment due upfront for services. This ensures prompt payment for any medical laboratory testing provided, reduces administrative overhead, and eliminates the need to deal with payers.
Concierge Medicine Is Not Just for the Wealthy Anymore
Since its inception, concierge care has been considered a luxury available to only financially well-off patients. However, that may soon change. Several major health systems and hospitals are piloting scaled-back versions of concierge care aimed at both middle- and upper-class consumers. However, the programs are not without critics and have elicited both positive and negative responses from healthcare providers.
According to Modern Healthcare, hospitals and health systems currently testing concierge care programs include:
Patients with busy schedules or chronic conditions may see the biggest gains from investing in concierge care. The added flexibility and increased access might allow them to take advantage of care options more frequently. Physicians being able to take their time during consultations and more closely focus on specific concerns is also seen as a benefit to patients.
However, Modern Healthcare points out that patients are not the only ones to see benefits from this arrangement.
“Doctors who have switched to concierge-style medicine sing its praises, claiming the smaller patient panel allows the doctor to build relationships with patients and spend more time on preventive medicine,” Modern Healthcare noted.
In 2016, Dark Daily reported on similar findings from the American Academy of Private Physicians (AAPP). They noted that the average primary care physician in the US maintained between 2,000 and 4,000 patients using the traditional care model. In contrast, the AAPP found concierge physicians maintained on average only 600 patients. (See, “Concierge Medicine Increases in Popularity as More Consumers Opt for This Care Model; Will Clinical Laboratories Exploit This Business Opportunity?” May 6, 2016.)
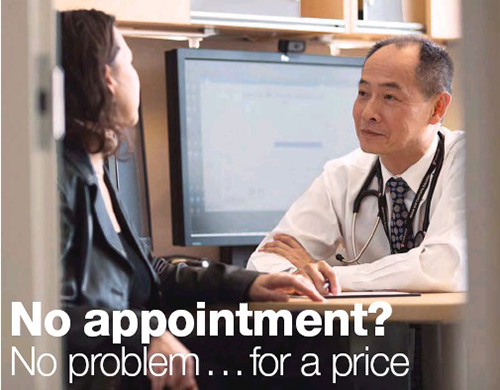
Paul Huang, MD, PhD (above right), a concierge doctor at Massachusetts General Hospital, told Modern Healthcare, “We are not doing this just to make more money—we are doing this to make money to put back into the mission of the hospital and to support programs that otherwise would be difficult to support.” (Photo copyright: Modern Healthcare.)
Concierge Care: Controversial Approach or Major Boon to Hospitals?
Since its debut in the 1990s, concierge care has faced scrutiny and opposition from those who feel it discriminates against those who cannot afford retainer premiums and out-of-pocket expenses.
One health system that has drawn such criticism is Michigan Medicine (MM), which is owned by the University of Michigan. As reported by the Detroit Free Press, in a letter to hospital administration, 200 of MM’s own doctors and staff expressed their feelings about the concierge care program, stating, “Victors Care purports to offer ‘better’ healthcare to those with enough money to pay a large access fee. The University of Michigan is a public institution and our commitment is to serve the public, not a private few. We do not feel this is the role of a state university and are unable to justify this to the patients and families we serve.”
Tom Cassels, a consulting partner with the Advisory Board Company, told Modern Healthcare, “It’s a cultural learning curve, because most not-for-profit health systems are geared toward providing the same level of service to everyone in their community. The fundamental model of concierge medicine is to price-discriminate.”
However, media coverage also highlights how the hospitals creating concierge care services are using the financial benefits to help offset the cost of low-margin services or provide care to low-income patients who wouldn’t otherwise have access to care.
Misty Hathaway, Senior Director of the Center for Specialized Services at Mass General, explained to Modern Healthcare that since their physicians are salaried, margins from concierge services can help support “things like our substance abuse program, or other parts of primary care where the margin is a little bit harder to achieve.”
Despite the ethical debates, use of concierge care services continues to gain momentum as middle and upper-class patients find the increased quality of care a worthy value proposition. As more options emerge at major healthcare centers, medical laboratories and other service providers might find that this trend also offers an opportunity to increase revenue with a minimal impact on administrative and billing costs.
—Jon Stone
Related Information:
Concierge Care Taking Hold at Some Large, Urban Hospitals
No Appointment? No Problem … For a Price
Exclusive U-M Medical Plan Buys You ‘Better’ Care, Special Access
The Future of Healthcare Could Be in Concierge Medicine
The Doctor Won’t See You Now
Concierge Medicine Increases in Popularity as More Consumers Opt for This Care Model; Will Clinical Laboratories Exploit This Business Opportunity?
More Doctors Consider Concierge Medicine as Healthcare Reform Looms
Concierge Medicine Trend Continues and Creates New Clients for Clinical Pathology Laboratories
Apr 4, 2018 | Laboratory Hiring & Human Resources, Laboratory Management and Operations, Laboratory News, Laboratory Operations, Laboratory Pathology, Management & Operations
Clinical laboratories may want to offset plunging patient lab specimens by increasing outreach business
Hospital admissions are in decline across the country and the trend is being blamed in part on the rising use of high-deductible health plans (HDHP). The implications for hospital-based clinical laboratories is that lower in-patient totals reduce the flow of patient lab specimens as well. This situation may encourage some hospital and health-system labs to increase their lab outreach business as a way to offset declining inpatient lab test volumes and help keep down overall average test costs.
Healthcare Dive, which named “changing patient admissions” its “Disruptor of the Year,” used data from America’s Health Insurance Plans (AHIP) annual surveys to show the admission rate trend that is causing hospital operators and health systems to rethink how they do business going forward.
“We are really talking about how providers are not taking in as much revenue as they are spending,” Healthcare Dive noted. “Hospitals are largely fixed cost businesses, and rising expenses have been outpacing admissions growth.”
Experts Claim the ‘Hand Writing Is on the Wall’
According to Healthcare Dive’s analysis of US hospital admissions, which used data from the American Hospital Association’s Annual Survey, hospital admissions peaked at 35.4 million in 2013, coinciding with the roll out of the Affordable Care Act. The total fell to 34.9 million in 2014, before rebounding slightly to 35.1 million in 2015. The 2016 survey, published in 2018, showed hospital admissions remaining relatively flat at approximately 35.2 million.

Paul Hughes-Cromwick (above), Co-Director, Sustainable Health Spending Strategies, Altarum in Ann Arbor, Mich., expects hospitals to be challenged by flat admission rates going forward. “Times are still pretty good, but the writing is on the wall for hospital operators,” he told Modern Healthcare. This will impact clinical laboratories owned by hospitals and health systems as well. Photo copyright: Long Beach Business Journal.)
Most experts place the blame for slumping patient admissions on HDHPs. Such plans, which are paired with a tax-advantaged health savings account, have enabled employers to shift initial medical costs to workers in exchange for lower monthly health insurance premiums. Nearly 20.2 million Americans were enrolled in HDHPs in 2016, up from 15.4 million in 2013 and far above the roughly one million plans in existence in 2005, the AHIP surveys revealed. HDHPs were first authorized by Congress in 2003.
Consumers Delaying or Opting Out of Healthcare
Faced with higher out-of-pocket medical costs, consumers are opting to postpone or forgo elective surgeries and procedures, which in turn is placing pressure on healthcare systems’ operating revenues.
According to Healthcare Dive, Community Health Systems experienced a 12% drop in operating revenue in the first nine months of fiscal year 2017, while HCA Healthcare and Tenet Healthcare dropped 6.7% and 3.8%, respectively.
J. Eric Evans, President of Hospital Operations, Tenet Healthcare (NYSE:THC), a 77-hospital chain, told Modern Healthcare, today’s consumers are spending their healthcare dollars differently.
“The more elective procedures, things like orthopedics, we see the softness,” Evans told Modern Healthcare. “So, we think that does play into the story of deductibles rising and changing behaviors.”
The challenges for not-for-profit hospital systems are no different. Modern Healthcare noted that the 14-hospital Indiana University Health system reported a 46% drop in operating income in the third quarter of FY 2017 on a year-over-year admission decline of 2%.
Healthcare Systems Rethinking Their Business Strategies
“Health systems en masse are reacting to shifting dynamics in healthcare utilization by throwing money and resources to lower cost settings, such as urgent care centers and freestanding emergency departments,” Healthcare Dive noted. Dark Daily has reported on this trend. (See, “From Micro-hospitals to Mobile ERs: New Models of Healthcare Create Challenges and Opportunities for Pathologists and Medical Laboratories,” May 26, 2017.) Health systems also are selling unprofitable hospitals and laying off or eliminating positions to cut costs. Tenet Healthcare, for example, is laying off 2,000 workers while selling eight of its US hospitals and all of its nine United Kingdom facilities, Modern Healthcare reported in January.
“We are seeing and are working with health systems to take out pretty significant amounts of cost out of their operations, both clinical and nonclinical, and setting targets like 15-20%, which is a transformative change,” Igor Belokrinitsky, Vice President and Partner at Strategy&, PricewaterhouseCoopers’ strategy consulting group, told Healthcare Dive in a 2017 interview.
Lower hospital in-patient volume means less clinical laboratory test orders. This, in turn, will result in increases in the average cost per inpatient test. Anatomic pathology groups and medical laboratory leaders who work in or service hospitals may wish to take proactive steps to boost test referrals from outpatient and outreach settings as a way to help keep down the lab’s average cost per test.
—Andrea Downing Peck
Related Information:
Disrupter of the Year: Softening Patient Admissions
Hospital Volumes Laid Low by High-Deductible Health Plans
How Hospitals Feel about AHCA’s Death, Future with ACA
2016 Survey of Health Savings Account-High Deductible Health Plans
Fast Facts on U.S. Hospitals, 2018
5 Things to Know about Tenet Healthcare’s Restructuring
From Micro-hospitals to Mobile ERs: New Models of Healthcare Create Challenges and Opportunities for Pathologists and Medical Laboratories
Mar 28, 2018 | Laboratory Hiring & Human Resources, Laboratory Instruments & Laboratory Equipment, Laboratory Management and Operations, Laboratory News, Laboratory Operations, Laboratory Pathology, Laboratory Testing, Management & Operations
Microhospitals already offer most of the critical features of traditional hospitals, and by featuring telemedicine technology at the point of care, they are becoming powerful tools for healthcare providers
Dark Daily reported in January that microhospitals are opening nationwide, including in such innovative states as Texas, Colorado, Nevada, and Arizona. In addition to being open 24/7 and mostly located in high-density areas, these scaled down hospitals feature the most critical aspects of full-size hospitals—medical laboratories, emergency departments, pharmacies, and imaging centers.
However, a report by the Health Resources and Service Administration (HRSA) predicted that by 2020 the US will be short as many as 20,000 primary care physicians! Many specialty practices also are expected to see stiff shortages of physicians in the near future. Without enough physicians, even microhospitals cannot provide adequate care.
Thus, the ever increasing practice of using telemedicine as a way to serve more people, while providing faster, more efficient care tailored to meet the needs of individuals and communities, is welcomed news. If this trend becomes more widespread, it will create new opportunities and challenges for clinical laboratories in hospitals, as well as health systems that own and operate microhospitals.
Filling a Need in Vulnerable Communities
At the end of 2016, there were approximately 50 microhospitals operating in the United States, mostly in the Midwest, Arizona, Colorado, Nevada, and Texas. Sometimes referred to as neighborhood or community hospitals, microhospitals are acute care facilities that are smaller than traditional hospitals but can deliver many of the same medical services. They provide more comprehensive treatments than typical urgent care and outpatient centers and fill a gap between freestanding healthcare centers and major hospitals.
Microhospitals typically have less than a dozen short-stay beds and have the ability to provide inpatient care, emergency care, and imaging and medical laboratory services. And, they are usually affiliated with larger healthcare systems, which allows them to expand into certain areas without incurring the high costs of building a full-scale hospital.
“Right now they seem to be popping up in large urban and suburban metro areas,” Priya Bathija, Vice President, Value Initiative American Hospital Association, told NPR. “We really think they have the potential to help in vulnerable communities that have a lack of access.”
Patient Satisfaction and Declining Physician Populations Drive Demand for Telemedicine
Telemedicine, a combination of telecommunications and information technology, is primarily used to remotely connect healthcare providers to patients during office visits. But it also is being used successfully at the point of care in emergency departments and even surgery.
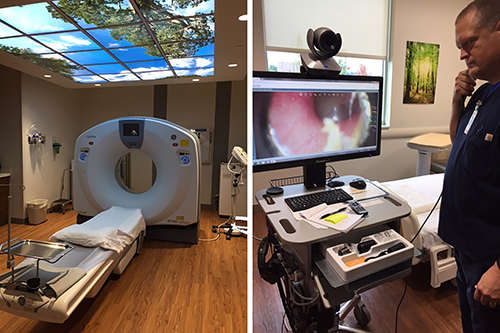
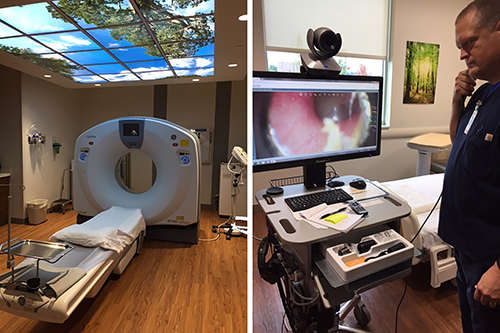
Microhospitals like St. Vincent Neighborhood hospital in Noblesville, Ind., which offer most of the critical functions of traditional hospitals, such as clinical laboratories, ERs, and the CT scanning station above (left), are increasingly including telemedicine technologies (above right) at the point of care to offset reductions in primary care and specialty physicians. (Photo copyright: Jill Sheridan/IPB News.)
Consumers are becoming more accepting of telemedicine (AKA, telehealth) as these services offer savings in both time and money. A recent survey by the Health Industry Distributors Association (HIDA) found that many patients were pleased with telehealth services. More than 50% of the surveyed individuals stated they were very satisfied with a recent telemedicine encounter. In addition, 54% of those individuals described their telehealth experience as better than a traditional, in-person office visit.
Telemedicine and Microhospitals Mutually Beneficial, According to HRSA
Other research suggests microhospitals may generate a mutually beneficial alliance with telemedicine that increases the progress of both entities, especially when considering projected increases in the number of nurse practitioners and physician assistants.
In its report, “Projecting the Supply and Demand for Primary Care Practitioners Through 2020,” Health Resources and Service Administration (HRSA) estimates there will be a shortage of more than 20,000 primary care physicians working in the US by the year 2020. Other specialties expected to experience staff shortfalls include:
Anticipation of this decline in physician numbers is fueling the demand for telemedicine to help with patient loads, especially in remote areas.
Saving Time and Money with Televisits
A study by Nemours Children’s Health System indicates that telemedicine may reduce medical costs for both patients and healthcare providers while sustaining patient satisfaction.
“At Nemours, we’ve seen how telemedicine can positively impact patients’ lives,” Shayan Vyas, MD, Medical Director of Telehealth at Nemours, noted in a press release. “The overwhelmingly positive response we’ve seen from parents who are early adopters of telemedicine really reinforces the feasibility of online doctor visits and sets the stage for real change in the way healthcare is delivered.”
The Nemours study involved 120 patients under the age of 18. The majority of families surveyed stated they would be interested in future telehealth visits and an impressive 99% said they would recommend telemedicine to other families.
The study discovered that patients and family members saved an average of $50 and about an hour of time, by utilizing telehealth for sports medicine appointments. The health system also experienced some monetary perks with the televisits, as they cost approximately $24 less per patient.
“We know that telemedicine is often looked to for common childhood ailments, like cold and flu, or skin rashes. But we wanted to look at how telemedicine could benefit patients within a particular specialty such as sports medicine,” Alfred Atanda Jr, MD, Pediatric Orthopedic Surgeon at Nemours/Alfred I. DuPont Hospital for Children in Wilmington, DE., told FierceHealthcare. “As the healthcare landscape continues to evolve and the emphasis on value and satisfaction continues to grow, telemedicine may be utilized by providers as a mechanism to keep costs and resource utilization low, and to comply with payer requirements.”
Healthcare consumers and providers are increasing looking to technology to enhance medical care and solve resource shortfalls. Separately, telehealth and microhospitals already help with these needs, Combined, however, they are a powerful solution to our nation’s reducing ranks of primary care physicians and medical specialists.
If this trend of microhospitals using telemedicine should continue and increase, both components will give medical professionals vital tools to provide faster, more economical, and more personalized services, to more patients across wider areas of America.
—JP Schlingman
Related Information:
Why Telehealth is Fueling the Move Towards Microhospitals
Projecting the Supply and Demand for Primary Care Practitioners Through 2020
Are Microhospitals the Answer for Systems Looking for Low-cost Expansions? They Might Be
Microhospitals: Healthcare’s Newest Patient Access Point
Microhospitals Could Prove Financial Boon and Salvation to Healthcare Systems
Microhospitals Provide Health Care Closer to Home
Telemedicine Saves Patients Time and Money, Study Shows
5 Common Questions about Micro-Hospitals, Answered
Survey: More than Half of Patients Prefer Telehealth Visits to In-Person Care
Majority of Parents Plan to Use Telemedicine for Pediatric Care
Microhospitals May Help Deliver Care in Underserved Areas
“Thinking Small” May Be Next Big Innovation in Healthcare Delivery as Microhospitals Spring Up in Metropolitan Areas Across Multiple States
Mar 5, 2018 | Compliance, Legal, and Malpractice, Laboratory Hiring & Human Resources, Laboratory News, Laboratory Pathology, Laboratory Testing
The indicted medical laboratory technician will also be required to pay back more than $69,000 to Hershey Medical Center
It what may be a unique first for the clinical laboratory industry, a medical technologist in Pennsylvania has been found guilty of a criminal felony for failing to perform certain cancer genetic tests according to approved protocols. The judge has sentenced the medical technologist to 15 months in prison and repayment of almost $70,000 in restitution.
Dark Daily reported on earlier developments in this case in 2017. Medical technologist Floyd Benko was indicted in 2015 after pleading guilty to false statement charges stemming from his work with genetic testing at Hershey Medical Center (HMC) between November 2014 and April 2015. Now, Benko has been sentenced to nearly 15 months in prison after pleading guilty to false statement charges.
US Middle District Judge Yvette Kane sentenced Benko to 15 months in prison with three years of supervised release following his prison term. He must also make restitution to HMC in the amount of $69,742 related to retesting of the gene mutation tests he previously performed in which the results were found to be inaccurate.
The sentence required Benko to report to the Pennsylvania Bureau of Prisons on January 22, 2018.
Failure to Follow Protocols Leads to Faulty Results and Eventual Sentencing
The charges levied against Benko relate to DNA gene mutation tests performed by him on behalf of HMC for 124 advanced-stage cancer patients. According to a Department of Justice press release, the genetic testing included:
“Benko failed to perform the assays in the manner called for by Hershey’s standard operating procedures,” the press release states. “Subsequent retesting of the patients during summer 2014, revealed that 60 of the 124 patients had assay results discordant with results obtained by two outside medical laboratories.”
Unusual Application of Federal Fraud Statute
Dark Daily’s previous coverage provides a detailed timeline of events leading up to Benko’s guilty plea.
Court filings state that in late 2013, a treating physician at HMC noted discordant results for tests when compared to a patient’s clinical profile. The physician resubmitted the test to an outside lab and received results that differed from those of Benko’s test.
This led to a request from HMC supervisors for Benko to repeat the test. Again, results differed from the outside laboratory. When supervisors asked for access to the tissue samples used for the test, Benko could not provide them.

Penn State Milton S. Hershey Medical Center (above) where in 2013 to 2014 Floyd Benko, a 60-year-old research technologist, improperly conducted 124 gene mutation clinical laboratory tests and then lied about it to cover up his lack of following standard operating procedures. (Photo copyright: PennLive/Paul Chaplin.)
Standard operating procedures (SOPs) for the tests in question—procedures Benko himself helped to create in conjunction with HMC—required preservation of all tissue samples. They also required the use of a Thermo Scientific NanoDrop 2000 spectrophotometer—a piece of equipment that Benko did not acknowledge using.
With Benko unable to provide samples, HMC triggered an FBI investigation into testing practices by Benko. The investigation yielded 125 tests for which samples were not preserved. Repeat testing by two outside medical laboratories—at HMC’s expense—resulted in 60 assay results returned that were discordant with Benko’s original findings.
Benko eventually resigned from HMC. He later attempted to explain the discordant results in two separate letters to HMC supervisors. However, in July 2015, a federal grand jury returned an indictment: one count of healthcare fraud and two counts of making false statements in healthcare matters to HMC.
Copies of court filings available at Leagle show that Benko initially disputed the charges using four primary arguments and requested case dismissal. These arguments were eventually denied by Kane. “In refusing to dismiss the charges against Benko, Kane rejected his arguments that his alleged actions don’t constitute a crime, especially since he didn’t profit financially,” noted PennLive. “The judge did, however, characterize the Benko case as an ‘unusual application of the federal healthcare fraud statute.’”
After denial of his dismissal, Benko entered a guilty plea to false statement charges in July 2017. Follow-up coverage from PennLive explained that Benko’s plea agreement included a stipulation that advised a sentence of up to 18 months—of which he received 15 months. At the time of sentencing, the final charge appears to be one count of making false statements.
Establishing Protocols and Ensuring Accuracy in Medical Laboratory Testing
Anatomic pathology and medical laboratory testing is an increasingly important part of the modern healthcare system. Both value-based care models and personalized medicine rely on lab results to help improve outcomes and tailor treatments to the individual patient profile.
By failing to follow SOPs when performing these clinical laboratory tests, Benko potentially jeopardized the treatment outcomes and health of more than 100 patients and also created liability concerns for the laboratory in which he was employed.
As highlighted by Benko’s sentence, the impact from this case was not limited to the lives of more than 100 patients. It also affected both the reputation of HMC and their financials—requiring nearly $70,000 in additional spending for the flawed assays—and to confirm the results of suspect tests performed by Benko. And, this does not account for the time and monetary costs related to the investigation and prosecution of the case, or public relations work surrounding the case.
As test volumes continue to increase and lab liability continues to take the spotlight, it is essential that clinical laboratories, anatomical pathology groups, and other diagnostic service providers maintain effective protocols and procedures to ensure the accuracy of test results. And they must establish comprehensive documentation and compliance programs that create accountability and highlight concerns quickly to ensure both patient and laboratory safety.
—Jon Stone
Related Information:
U.S. v. BENKO No. 1:15-cr-00159
Former Hershey Medical Center Worker Pleads Guilty to Lying About Cancer Testing Procedure
Judge Won’t Dismiss Charges That Hershey Med Tech Fudged Genetic Tests for Cancer Patients
Former Hershey Medical Center Research Technologist Sentenced for Making False Statements About Cancer Tests
Penn State University College of Medicine (COM); The Penn State Hershey Medical Center (PSHMC): Standard Operating Procedures (SOPs) Regarding Review and Management of Conflict of Interest
Hershey, Pennsylvania, Clinical Laboratory Technician Indicted in 2015 for Fraudulent Cancer Test Results Pleads Guilty to False Statement Charges