Dec 7, 2018 | Compliance, Legal, and Malpractice, Laboratory Management and Operations, Laboratory News, Laboratory Operations, Laboratory Pathology, Laboratory Testing
Experts say medical laboratories must overcome staffing challenges and develop a culture of continual inspection readiness
Clinical laboratories and anatomic pathology groups will be entering 2019 facing not only financial upheaval from Medicare Part B fee cuts and narrowing payer networks, but also an increasingly rigorous and ever-evolving regulatory environment.
Although the Clinical Laboratory Improvement Amendments (CLIA) requirements have not undergone major changes since debuting in 1992, the medical laboratory industry has become more complex and technology-laden, resulting in old rules being applied to emerging technologies.
“People can get lulled into this sense that we know what standards are and we’re meeting them, but what has happened is the rules haven’t really changed—the industry has,” says Nora L. Hess, MBA, MT(ASCP), Senior Consultant for Accumen, a lab quality improvement company in San Diego, CA. “Technology is now jumping ahead so fast that keeping up with it and understanding how the rules are going to be applied is challenging.”
Hess and Anne T. Daley, MS, Quality Officer at ARUP Laboratories in Salt Lake City, UT, will co-present a 90-minute webinar on Dec. 13th titled, “Make Your Lab Assessment Ready in 2019: Know the Most Common Deficiencies in Accreditation and Certification and What to Expect in the Future.”
The program will review the top deficiencies reported by the College of American Pathologists (CAP), the Joint Commission, A2LA, and COLA.

Anne T. Daley, MS, CMQOE, CSSBB, CLC, MT, DLM (left), and Nora L. Hess, MBA, MT(ASCP), PMP (right), are Senior Consultants with Chi Solutions, an Accumen company. Together, they have extensive first-hand experience guiding clinical laboratories through the rigid and rigorous process of achieving inspection-ready status. (Photo copyrights: Chi Solutions, Inc.)
Why being ‘Inspection Ready’ Can Improve Performance and Increase Revenue
Striving to be “inspection ready” should be the goal of every clinical laboratory and pathology group. However, Daley notes labs typically operate with staffs that are stretched thin by retirements, illnesses, staff shortages, or ancillary demands on administrators’ time, caused by system-wide initiatives that range from electronic health record (EHR) rollouts to integration and consolidation of other labs.
“Most hospital laboratories are staffed at a level where they are working hard just to meet the daily patient care needs,” Daley says. “You add in all these additional projects and something has to give.”
In today’s challenging environment, Hess says laboratories that consistently perform well during the inspection process share several characteristics, including the following:
- a culture of quality across the laboratory; and,
- an emphasis on inspection readiness.
“They make inspection readiness a consistent focus across the entire laboratory,” Hess notes. “It becomes part of the calendar. It becomes part of what they talk about all the time. It is a part of their decision-making. It is hardwired into who they are and what they do … successful laboratories are making this part of their day-to-day activities, so it doesn’t get lost in the shuffle and it doesn’t get back-burnered.”
Hess and Daley note the types of deficiencies cited by accreditation agencies tend not to vary much from year to year. Testing personnel competency and proficiency testing are common themes, annually ranking high on top-10 lists of deficiencies found. However, laboratory directors increasingly are being singled out for issues related to qualifications and performance of responsibilities.
(To register for their Dec. 13th webinar or to order a DVD, click here. Or, copy and paste this URL into your browser: https://www.darkdaily.com/webinar/make-your-lab-assessment-ready-in-2019-know-the-most-common-deficiencies-in-accreditation-and-certification/).
—Andrea Downing Peck
Related Information:
Make Your Lab Assessment Ready in 2019: Know the Most Common Deficiencies in Accreditation and Certification
CLIA Inspection–What they Mean and How to Avoid Them
‘We Wanted to Be the Best we Could Possibly Be’: CAP ISO 15189-Accredited Labs on the Difference it Makes
Are CLIA Inspections of Clinical Pathology Laboratories Getting Tougher? Why It Pays to Achieve “Inspection Readiness”
Nov 28, 2018 | Digital Pathology, Instruments & Equipment, Laboratory Instruments & Laboratory Equipment, Laboratory Management and Operations, Laboratory News, Laboratory Operations, Laboratory Pathology, Laboratory Testing
Clinical laboratory leaders aiming for patient-centered care and precision medicine outcomes need to acknowledge that patients do not want to be in hospitals or travel to physician offices and patient care centers for blood tests. It can be inconvenient, sometimes costly, and often painful.
That’s why disease management methods such as remote patient monitoring are appealing to many people. It’s a big market estimated to reach $1 billion by 2020, according to a Transparency Market Research Report. The study also associated popularity of devices such as heart rate and respiratory rate monitors with economic pressures of unnecessary hospital readmissions.
But can remote patient monitoring be used for more than to check heart rates, monitor blood glucose, and track activity levels? Could such technology be effectively leveraged by medical laboratories for remote blood sampling?
Microsampling versus Dried Blood Collecting
Remote patient monitoring must be able to address a large number of diseases and chronic health conditions for it to continue to expand and gain acceptance as a viable way to care for patients in different settings outside of hospitals. However, as most clinical pathologists and laboratory scientists know, clinical laboratory testing has an essential role in patient monitoring. Thus, there is the need for a way to collect blood and other relevant samples from patients in these remote settings.
One promising approach is the development of new microsampling technology that can overcome past obstacles of dried blood collection. Furthermore, microsampling-enabled devices can make it possible for medical laboratories to reach out to the homebound to secure accurate and volumetrically appropriate samples in a cost-effective manner.
“One well-established fact in today’s healthcare system is that an ever-greater proportion of patients want clinical care that is less invasive and less intrusive,” noted Robert Michel, Editor-in-Chief of Dark Daily and The Dark Report. “Patients want to take more control over their treatment and be more effective at maintaining the stability of their chronic conditions, and often are happier than those who need to travel to have chronic conditions monitored. To meet this need there has been significant innovation, particularly in the area of remote blood sampling using microsampling technology.”
For decades, medical laboratories have tried various methods for acquiring and transporting blood samples from remote locations. One such non-invasive alternative to venipuncture is called dried blood spot (DBS) collecting. It involves placing a fingerprick of blood on filter paper and allowing it to dry prior to transport to the lab.
But DBS collected bio samples often do not contain enough hematocrit (volume percentage of red blood cells) for laboratories and clinical pathologists to provide accurate reports and interpretations. Reported reasons DBS cards have not penetrated a wide market include:
- Hematocrit bias or effect;
- Costly card punching and automation equipment; and,
- Possible disruption to existing lab workflows.
Microsampling Technology Enables Collection of Appropriate Samples
Microsampling has to have the capability to enable labs to deliver quality results from reliable blood samples. This remote sampling technology makes it possible for phlebotomists to offer a comfortable collection alternative for homebound patients and rural residents. It also can be useful for physicians stationed in remote areas. Patients themselves can even collect their own blood samples.
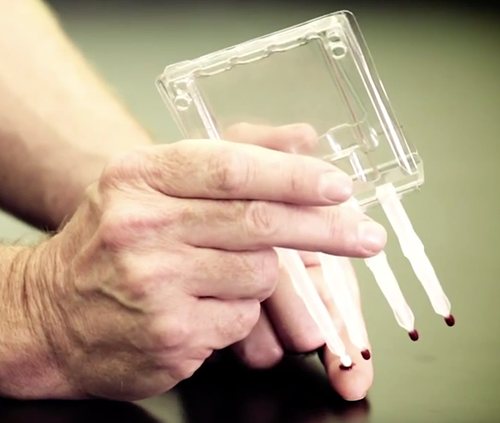
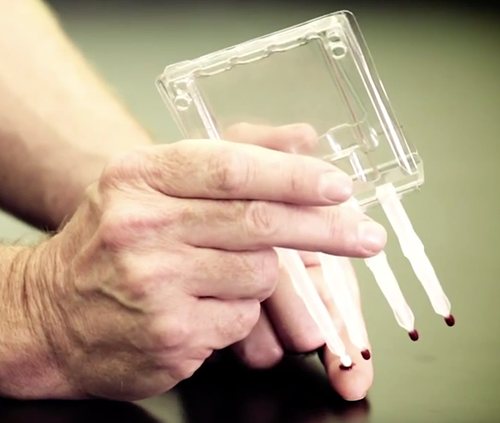
Volumetric Absorptive Microsampling (VAMS) technology enables accurate samples of blood or other fluids from amounts as small as 10, 20, or 30 microliters, according to Neoteryx, LLC, of Torrance, Calif., the developer of VAMS. The technology is integrated into the company’s Mitra microsampler blood collection devices (shown above) in formats for patient use and for medical laboratory microsample accessioning and extraction. Click here to watch a video on the Mitra Microsampler Specimen Collection Device. (Photo copyright: Neoteryx.)
One company developing these types of products is Neoteryx, LLC, of Torrance, Calif. It develops, manufactures, and distributes microsampling products. Patients with the company’s Mitra device use a lancet to puncture their skin and draw a small amount of blood, collect it on the device’s absorptive tip, and then mail the samples to a blood lab for testing (Neoteryx does not perform testing).

“Technologies such VAMS are driving [precision medicine] in an extremely cost-effective manner, while only requiring minimal patient effort. Patients are taking a more active role in their healthcare journeys, and at-home sampling is supporting this shift,” stated Fasha Mahjoor, Chief Executive Officer, Neoteryx, in a blog post. (Photo copyright: Neoteryx.)
Patient satisfaction survey data collected by Neoteryx suggest patients are comfortable with their role in blood collection:
- 70% are comfortable or very comfortable with the process;
- 86% say it is easy or very easy to use the Mitra device;
- 92% report it is easy to capture blood on the device’s tip;
- 55% of Mitra device users are likely or very likely to choose microsampling over traditional venipuncture; and,
- 93% noted they are likely or very likely to choose the device for child care.
A list of published studies describes certain advantages of VAMS technology that have implications for medical laboratories and clinical pathologists:
- Microsampling has benefits and implications for therapeutic drug monitoring, infectious disease research, and remote specimen collection;
- Dried blood microsamples from fingerstick can generate reliable data “correlating” to traditional blood collection processes;
- Bioanalytical data collected with the Mitra device are accurate and dependable; and,
- In a study for a panel of anti-epileptic drugs, VAMS led to optimized extraction efficiency above 86%, which means there was no hematocrit bias.
Learn More by Requesting the Dark Daily Microsampling White Paper
To help medical laboratories and clinical pathologists learn more about microsampling and VAMS devices, Dark Daily and The Dark Report have produced a white paper titled “How to Create a Patient-Centered Lab with Breakthrough Blood Collection Technology: Microsampling Takes Blood Collection Out of the Clinic.” The paper includes sections addressing these topics:
- Rise of patient-centered care and remote patient monitoring;
- Dried blood collection over the years and the hematocrit effect;
- A look at microsampling and how it takes blood collection out of the clinic;
- How Volumetric Absorptive Microsampling (VAMS) technology works;
- Patient satisfaction data;
- Research about microsampling including extensive graphics;
- Launching new VAMS technology; and,
- Frequently asked questions.
Innovative medical laboratory leaders who want to increase their understanding of how microsampling technology and remote patient monitoring relates to the goal of becoming a patient-centered lab are encouraged to request a copy of the white paper. It can be downloaded at no cost by clicking here, or placing https://www.darkdaily.com/how-to-create-a-patient-centered-lab-with-breakthrough-blood-collection-technology-9-2018/ into your browser.
—Donna Marie Pocius
Related Information:
Remote Patient Monitoring Devices Market
Neoteryx, LLC, and Cedars Sinai Partner to Investigate at Home Blood Sampling Possibilities for Patients with Inflammatory Bowel Disease
Creating a Patient-Centered Lab with Breakthrough Blood Collection Technology Using New Microsampling Methods Provides Reliable, Economic Collection, Shipping and Storage Solutions
How to Create a Patient-Centered Lab with Breakthrough Blood Collection Technology: Microscopy Takes Blood Collection Out of the Clinic
Nov 26, 2018 | Coding, Billing, and Collections, Instruments & Equipment, Laboratory News, Laboratory Operations, Laboratory Pathology, Laboratory Testing, Management & Operations
Despite the widespread adoption of electronic health record (EHR) systems and billions in government incentives, lack of interoperability still blocks potential benefits of digital health records, causing frustration among physicians, medical labs, and patients
Clinical laboratories and anatomic pathology groups understand the complexity of today’s electronic health record (EHR) systems. The ability to easily and securely transmit pathology test results and other diagnostic information among multiple providers was the entire point of shifting the nation’s healthcare industry from paper-based to digital health records. However, despite recent advances, true interoperability between disparate health networks remains elusive.
One major reason for the current situation is that multi-hospital health systems and health networks still use EHR systems from different vendors. This fact is well-known to the nation’s medical laboratories because they must spend money and resources to maintain electronic lab test ordering and resulting interfaces with all of these different EHRs.
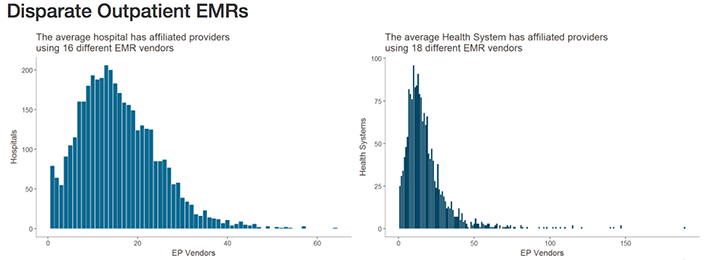
Healthcare IT News highlighted the scale of this problem in recent coverage. Citing data from the Healthcare Information and Management Systems Society (HIMSS) Logic database, they note that—when taking into account affiliated providers—the typical health network engages with as many as 18 different electronic medical record (EMR) vendors. Similarly, hospitals may be engaging with as many as 16 different EMR vendors.

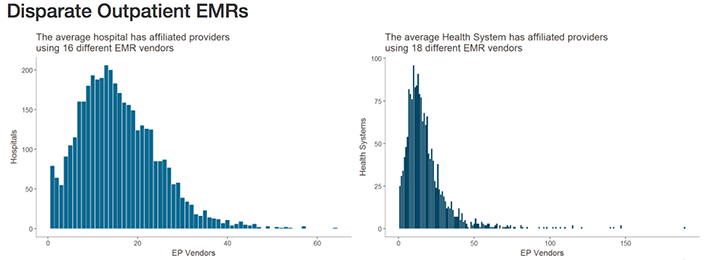
The graphics above illustrates why interoperability is the most important hurdle facing healthcare today. Although the shift to digital is well underway, medical laboratories, physicians, and patients still struggle to communicate data between providers and access it in a universal or centralized manner. (Images copyright: Healthcare IT News.)
The lack of interoperability forces healthcare and diagnostics facilities to develop workarounds for locating, transmitting, receiving, and analyzing data. This simply compounds the problem.
According to a 2018 Physician’s Foundation survey, nearly 40% of respondents identified EHR design and interoperability as the primary source of physician dissatisfaction. It has also been found to be the cause of physician burnout, as Dark Daily reported last year in, “EHR Systems Continue to Cause Burnout, Physician Dissatisfaction, and Decreased Face-to-Face Patient Care.”
Pressure from Technology Giants Fuels Push for Interoperability
According to HITECH Answers, the Centers for Medicare and Medicaid Services (CMS) has paid out more than $38-billion in EHR Incentive Program payments since April 2018.
Experts, however, point out that government incentives are only one part of the pressure vendors are seeing to improve interoperability.
“There needs to be a regulatory push here to play referee and determine what standards will be necessary,” Blain Newton, Executive Vice President, HIMSS Analytics, told Healthcare IT News. “But the [EHR] vendors are going to have to do it because of consumer demand, as things like Apple Health Records gain traction.”
Dark Daily covered Apple’s progress into organizing protected health information (PHI) and personal health records (PHRs) earlier this year in, “Apple’s Update of Its Mobile Health App Consolidates Data from Multiple EHRs and Makes It Easier to Push Clinical Laboratory Data to Patients.” It is one of the latest examples of Silicon Valley tech companies attempting to jump into the health sector and providing patients and consumers access to the troves of medical data created in their lifetime.
Another solution, according to TechTarget, involves developing application programming interfaces (APIs) that allow tech companies and EHR vendors to achieve better interoperability by linking information in a structured manner, facilitating secure data transmission, and powering the next generation of apps that will bring interoperability ever closer to a reality.
TechTarget reported on how University of Utah Hospital’s five hospital/12 community clinic health network, and Intermountain Healthcare, also in Utah, successfully used APIs to develop customized interfaces and apps to improve accessibility and interoperability with their Epic and Cerner EHR systems.
Diagnostic Opportunities for Clinical Laboratories
As consumers gain increased access to their data and healthcare providers harness the current generation of third-party tools to streamline EHR use, vendors will continue to feel pressure to make interoperability a native feature of their EHR systems and reduce the need to rely on HIT teams for customization.
For pathology groups, medical laboratories, and other diagnosticians who interact with EHR systems daily, the impact of interoperability is clear. With the help of tech companies, and a shift in focus from government incentives programs, improved interoperability might soon offer innovative new uses for PHI in diagnosing and treating disease, while further improving the efficiency of clinical laboratories that face tightening budgets, reduced reimbursements, and greater competition.
—Jon Stone
Related Information:
Why EHR Data Interoperability Is Such a Mess in 3 Charts
EHR Incentive Program Status Report April 2018
New FDA App Streamlines EHR Patient Data Collection for Researchers
AAFP Nudges ONC toward EHR Interoperability
A New Breed of Interoperable EHR Apps Is Coming, but Slowly
Top Interoperability Questions to Consider during EHR Selection
EHR Design, Interoperability Top List of Physician Pain Points
2018 Survey of America’s Physicians: Practice Patterns & Perspectives
ONC: 93% of Hospitals Have Adopted Most Recent EHR Criteria, but Most Lag in Interoperability
Open Standards and Health Care Transformation: It’s Finally Delivering on the Value It Promised
Apple’s Update of Its Mobile Health App Consolidates Data from Multiple EHRs and Makes It Easier to Push Clinical Laboratory Data to Patients
EHR Systems Continue to Cause Burnout, Physician Dissatisfaction, and Decreased Face-to-Face Patient Care
Nov 23, 2018 | Laboratory Management and Operations, Laboratory News, Laboratory Operations, Laboratory Pathology, Laboratory Testing, Management & Operations
PwC report indicates deal-making may generate long-term savings, but adds to higher medical costs as hospital systems dominate markets and drive up prices
Consolidation of big hospital health networks combined with a loss of independent doctor practices has changed the healthcare landscape in recent years, and clinical laboratories and anatomic pathology groups have been directly impacted. Now, those trends, along with increased access to care, are expected to push employer medical cost up by as much as 6% in 2019.
That’s according to the PricewaterhouseCoopers (PwC) Health Research Institute (HRI) “Behind the Numbers” annual analysis of the employer-based market.
The continued deal-making is bad news for medical laboratories, since super-sized hospital systems typically trim the budgets of laboratory and other services to improve operating efficiencies.
At the same time, more doctors are practicing as employees of hospitals, health networks, and medical groups. This physician consolidation presents challenges for independent clinical laboratories, which often lose test orders to in-house hospital labs when physicians no longer practice independently.
Consumer Demand for Access to Healthcare Will Drive Costs Higher
Consolidation-related pressures are not the only forces pushing medical costs higher. HRI expects a third factor to inflate medical costs in 2019—consumer pressure for more ways to access care.
The growth of care options such as: retail clinics, telemedicine, urgent care, and on-site employer health clinics may bring prices down over time, however increased utilization often raises employers’ healthcare costs in the short-term as workers take advantage of easier ways to access care, the report states.
Less Flu and High-Performing Health Networks Expected to Lower Costs
Conversely, HRI believes a milder flu season in 2018-2019 may help keep spending increases in check. Additionally, the growing number of healthcare advocates in the workplace who educate employees on the use of their healthcare benefits, plus the creation of high-performing health networks—both of which emphasize high-quality care alongside cost savings—should serve to deflate healthcare spending.
In an interview with FierceHealthcare, Barbara Gniewek, a Health Services Principal at PwC, compared attempts to control healthcare spending to a balloon. “Every time you squeeze one area” another issue crops up, she said.
Employer healthcare costs have risen 5.5% to 7% annually for each of the past five years. HRI contends downward pressure on healthcare prices overall—not just drug prices—may be the only remaining way for employers and health plans to keep healthcare spending from outpacing inflation.
“Efforts by employers to cut utilization have mostly run their course,” the report states. “Employers and consumers are plagued by high prices that continue to grow because of new, expensive medical services and drugs, and other factors, such as consolidation.”
While the 2019 spending number pales in comparison to the annual double-digit growth in healthcare spending two decades ago, Gniewek told RevCycleIntelligence the inflation news should not be viewed as positive.

“While some people are relieved that it’s not the high rates of 15 or 20 years ago, costs going up at that rate still [are] unsustainable,” Barbara Gniewek, Health Services Principal at PwC, told RevCycleIntelligence. “We still haven’t figured out how to control healthcare costs and we still don’t have the type of healthcare that we need.” (Photo copyright: PricewaterhouseCoopers.)
In theory, healthcare consolidation should create economies of scale that result in efficiencies that drive costs lower. However, reality can be much different, since short-term prices often rise when one health system suddenly dominates a market.
“We need to start getting to the point where we pull out the excess redundancies in the system and be able to monetize that in terms of savings,” Gniewek told RevCycleIntelligence. “We just haven’t seen that happen yet. It’s been more, ‘I own the market, so I can drive up the prices.’ As the government and employers demand better price control and want to do some direct contracting or high-performing networks, then eventually consolidations will be more efficient.”
Knowledge@Wharton, an online business analysis journal from the Wharton School of the University of Pennsylvania, notes one of the consequences of the Affordable Care Act was the “giant wave of consolidation” it sparked.
“It’s both ‘horizontal’ and ‘vertical,’ meaning hospitals aren’t just buying other hospitals, they’re picking up physician practices, rehabilitation facilities, and other ancillary healthcare providers,” a Knowledge@Wharton article on hospital consolidation stated.
Of the 115 health-system and hospital mergers announced in 2017, 10 were mega-deals involving sellers with net annual revenues of at least $1 billion, PwC noted in its annual report. The largest is a $28.4 billion merger between San Francisco-based Dignity Health and Catholic Health Initiatives of Englewood, Colo., which is expected to close in the coming year, according to a press release.
And a July 2018 report from the National Council on Compensation Insurance (NCCI) notes that though hospital mergers can lead to operating cost reductions for acquired hospitals of 15% to 30%, those reductions usually do not translate into price decreases.
“Research to date shows that hospital mergers increase the average price of hospital services by 6% to 18%. For Medicare, hospital concentration increases costs by increasing the quantity of care, rather than the price of care,” NCCI stated.
Clinical Laboratories May Be Part of Cost Reductions
The impact of physician employment was underscored in the March 2018 update to the Physician Advocacy Institute’s “Physician Practice Acquisition Study: National and Regional Changes in Physician Employment 2012-2016.” Over a four-year period from July 2012 to July 2016, the percentage of hospital-employed physicians increased by more than 63%.
If the factors fueling today’s increases in healthcare spending—consolidation and convenience—continue pushing costs higher, clinical laboratories and anatomic pathology groups will most likely be impacted as employers, insurers, and consumers look for ways to cut medical costs.
In this environment, medical laboratories must continually work to deliver more value to providers, patients, and healthcare networks.
—Andrea Downing Peck
Related Information:
Medical Cost Trend: Behind the Numbers 2019
Report: Consolidation, Convenience Care Major Drivers Behind Increased Healthcare Costs in 2019
The Impact of Hospital Consolidation on Medical Costs
Dignity Health and Catholic Health Initiatives to Combine to Form New Catholic Health System Focused on Creating Healthier Communities
Updated Physician Practice Acquisition Study: National and Regional Changes in Physician Employment 2012-2016
Healthcare Mergers, Increased Access to Boost Medical Costs 6%
Nov 19, 2018 | Laboratory Management and Operations, Laboratory News, Laboratory Operations, Laboratory Pathology, Laboratory Testing, Management & Operations
New bioinformatic tool finds gut microbiota may be ‘potential reservoir of bloodstream pathogens’ suggesting patients’ own bodies can be source of infections
Clinical laboratories in hospitals and health networks throughout the nation are collaborating in the priority effort to reduce deaths from sepsis and related blood infections. Now comes news that researchers at Stanford have identified an unexpected source of bloodstream infections. This finding may help medical laboratories contribute to faster and more accurate diagnoses of blood infections, particularly for hospital inpatients.
Lax infection-control practices often are blamed for hospital-acquired infections (HAIs). And HAIs certainly have been responsible for many tragic avoidable deaths. However, new research from Stanford University School of Medicine shows that hospital staff, other patients, or unclean instruments may not be solely responsible for all infections that present during hospital stays. According to Stanford researchers, a patient’s own digestive tract can be the surprising culprit for many bloodstream infections. This finding confirms a common belief that the patient’s microbiome probably is involved in many blood infections.
Clinical pathologists have become vital players in infection prevention programs, as hospitals intensify their focus on reducing HAIs. That’s especially in light of the Centers for Medicare and Medicaid Services (CMS) implementation of the pay-for-performance Hospital-Acquired Condition (HAC) Reduction Program. Now, Stanford researchers have found that for many hospital patients their own bodies may be the source of infections.
The researchers published their findings in Nature Medicine.
Bacteria Causing Blood Infections Found in Patients’ Stool Samples After Bone Marrow Transplants
Using a new bioinformatic computational tool called StrainSifter, the Stanford University team rapidly and accurately identified a surprising infection source in a group of hospitalized patients—microbes already living in the patients’ large intestines—a Stanford University news release explained.
The researchers analyzed blood and stool samples from 30 patients who developed bloodstream infections after receiving bone marrow transplants between October 2015 and June 2017 at Stanford Hospital. The researchers sought to determine whether the bacteria isolated from the patients’ blood also was found in stool specimens that had been collected prior to the transplants. The process required sequencing not only the patients’ DNA, but also analyzing the genomes of all the individual microbial strains resident in each patient’s stool.

“Just finding E. coli in a patient’s blood and again in the patient’s stool doesn’t mean they’re the same strain,” Ami Bhatt, MD, PhD, Assistant Professor of Hematology and Genetics at Stanford, explained in the news release. Bhatt served as senior author of the study. (Photo copyright: Stanford University.)
Analysis found that more than one-third of the patients’ stool samples (11) contained detectable levels of the same bacterial strain that had caused those patients’ bloodstream infections.
“Because the gut normally harbors more than 1,000 different bacterial strains, it’s looked upon as a likely culprit of bloodstream infections, especially when the identified pathogen is one known to thrive inside the gut,” Ami Bhatt, MD, PhD, Assistant Professor of Hematology and Genetics at Stanford, said in the news release. “But while this culpability has been assumed—and it’s an entirely reasonable assumption—it’s never been proven. Our study demonstrates that it’s true.”
Clinical and DNA data confirmed the gastrointestinal presence of Escherichia coli and Klebsiella pneumonia, common causes of pneumonia, urinary tract infections, and other potentially serious conditions. In addition, they found other disease-causing pathogens in the gut that they would not have expected to be there.
“We also find cases where typically nonenteric [outside the intestine] pathogens, such as Pseudomonas aeruginosa and Staphylococcus epidermidis, are found in the gut microbiota, thereby challenging the existing informal dogma of these infections originating from environmental or skin sources,” Fiona Tamburini, a senior graduate student, and postdoctoral scholar Tessa Andermann, MD, MPH, Infectious Disease Medical Fellow, wrote in Nature Medicine.
New Tool for Precision Medicine
Bhatt believes being able to trace the source of bloodstream infections will help doctors provide more targeted treatments for HAIs and potentially lead to effective prevention methods. This will create a new opportunity for microbiology laboratories to provide the necessary diagnostic tests designed to guide therapeutic choices of attending physicians.
“Until now, we couldn’t pinpoint those sources with high confidence,” Bhatt said in the news release. “That’s a problem because when a patient has a bloodstream infection, it’s not enough simply to administer broad-spectrum antibiotics. You need to treat the source, or the infection will come back.”
Bhatt says the computational tool has the potential to allow medical practitioners to quickly identify whether a pathogen responsible for a patient’s bloodstream infection came from a break in the skin, leaked through the intestinal wall into the blood, or was passed on through an inserted catheter or other object.
Bhatt’s team focused on the intestines for their study because it’s the home of 1,000 to 2,000 different germs. Dark Daily has reported often on developments involving human gut bacteria (AKA, microbiome) in e-briefings going back to 2013. While these gut bacteria do not typically cause problems, Bhatt said, “It’s only when they show up in the wrong place—due, for example, to leaking through a disrupted intestinal barrier into the bloodstream—that they cause trouble.”
Because nearly 40% of immunocompromised patients who spend up to six weeks in a hospital develop bloodstream infections, the Stanford findings could signal a major breakthrough in preventing HAIs. However, larger studies are needed to validate the researchers’ contention that the gut is a “potential reservoir of bloodstreams pathogens.”
If true, microbiologists and clinical pathologists may in the future have a new method for helping hospitals identify, track, and treat blood-born infections as well as and preventing HAIs.
—Andrea Downing Peck
Related Information:
Study Traces Hospital-Acquired Bloodstream Infections to Patients’ Own Bodies
Hospital-Acquired Condition Reduction Program Fiscal Year 2019 Fact Sheet
Precision Identification of Diverse Bloodstream Pathogens in the Gut Microbiome
Multiple Dark Daily E-briefings on Human Gut Bacteria (Microbiome)
Nov 16, 2018 | Digital Pathology, Instruments & Equipment, Laboratory Instruments & Laboratory Equipment, Laboratory Management and Operations, Laboratory News, Laboratory Operations, Laboratory Pathology, Laboratory Testing
New study conducted by an international team of researchers suggests that artificial intelligence (AI) may be better than highly-trained humans at detecting certain skin cancers
Artificial intelligence (AI) has been working its way into health technology for several years and, so far, AI tools have been a boon to physicians and health networks. Until now, though, the general view was that it was a supplemental tool for diagnosticians, not a replacement for them. But what if the AI was better at detecting disease than humans, including anatomic pathologists?
Researchers in the Department of Dermatology at Heidelberg University in Germany have concluded that AI can be more accurate at identifying certain cancers. The challenge they designed for their study involved skin biopsies and dermatologists.
They pitted a deep-learning convolutional neural network (CNN) against 58 dermatologists from 17 countries to determine which was more accurate at detecting malignant melanomas—humans or AI. A CNN is an artificial network based on the biological processes that occur when neurons in the brain are connected to each other and respond to what the eye sees.
The CNN won.
“For the first time we compared a CNN’s diagnostic performance with a large international group of 58 dermatologists, including 30 experts. Most dermatologists were outperformed by the CNN. Irrespective of any physicians’ experience, they may benefit from assistance by a CNN’s image classification,” the report noted.
The researchers published their report in the Annals of Oncology, a peer-reviewed medical journal published by Oxford University Press that is the official journal of the European Society for Medical Oncology.

“I expected only a performance on an even level with the physicians. The outperformance even of the average experienced and trained dermatologists was a major surprise,” Holger Haenssle, PhD, Professor of Dermatology at Heidelberg University and one of the authors of the study, told Healthline. Anatomic pathologists will want to follow the further development of this research and its associated diagnostic technologies. (Photo copyright: University of Heidelberg.)
Does AI Tech Have Superior Visual Acuity Compared to Human Eyes?
The dermatologists who participated in the study had varying degrees of experience in dermoscopy, also known as dermatoscopy. Thirty of the doctors had more than five-year’s experience and were considered to be expert level. Eleven of the dermatologists were considered “skilled” with two- to five-year’s experience. The remaining 17 doctors were termed beginners with less than two-year’s experience.
To perform the study, the researchers first compiled a set of 100 dermoscopic images that showed melanomas and benign moles called Nevi. Dermoscopes (or dermatoscopes) create images using a magnifying glass and light source pressed against the skin. The resulting magnified, high-resolution images allow for easier, more accurate diagnoses than inspection with the naked eye.
During the first stage of the research, the dermatologists were asked to diagnose whether a lesion was melanoma or benign by looking at the images with their naked eyes. They also were asked to render their opinions for any needed action, such as surgery and follow-up care based on their diagnoses.
After this part of the study, the dermatologists on average identified 86.6% of the melanomas and 71.3% of the benign moles. More experienced doctors identified the melanomas at 89%, which was slightly higher than the average of the group.
The researchers also showed 300 images of malignant and benign skin lesions to the CNN. The AI accurately identified 95% of the melanomas by analyzing the images.
“The CNN missed fewer melanomas, meaning it had a higher sensitivity than the dermatologists, and it misdiagnosed fewer benign moles as malignant melanoma, which means it had a higher specificity. This would result in less unnecessary surgery,” Haenssle told CBS News.
In a later part of the research, the dermatologists were shown the images a second time and provided clinical information about the patients, including age, gender, and location of the lesion. They were again instructed to make diagnoses and projected care decisions. With the additional information, the doctors’ average detection of melanomas increased to 88.9% and their recognition of benign moles increased to 75.7%. Still below the results of the CNN.
These findings suggest that the visual pattern recognition of AI technology could be a meaningful tool to help physicians and researchers diagnose certain cancers.
“In the future, I think AI will be integrated into practice as a diagnostic aide, particularly in primary care, to support the decision to excise a lesion, refer, or otherwise to reassure that it is benign,” Victoria Mar, PhD, an Adjunct Senior Lecturer in the Department of Public Health and Preventative Medicine at Australia’s Monash University, told Healthline.
“There is the potential for AI technology to be integrated with 2D or 3D skin imaging systems, which means that the majority of benign lesions would be already filtered by the machine, so that we can spend more time concentrating on the difficult or more concerning lesions,” she said. “To me, this means a more productive interaction with the patient, where we can focus on appropriate management and provide more streamlined care.”
AI Performs Well in Other Studies Involving Skin Biopsies
This study is not the only research that suggests entities besides humans may be utilized in diagnosing some cancers from images. Last year, computer scientists at Stanford University performed similar research and found comparable results. For that study, the researchers created and trained an algorithm to visually diagnose potential skin cancers by looking at a database of skin images. They then showed photos of skin lesions to 21 dermatologists and asked for their diagnoses based on the images. They found the accuracy of their AI matched the performance of the doctors when diagnosing skin cancer from viewed images.
And in 2017, Dark Daily reported on three genomic companies developing AI/facial recognition software that could help anatomic pathologists diagnose rare genetic disorders. (See, “Genomic Companies Collaborate to Develop Facial Analysis Technology Pathologists Might Eventually Use to Diagnose Rare Genetic Disorders,” August 7, 2017.)
While many dermatologists read patient biopsies on their own, they also refer high volumes of skin biopsies to anatomic pathologists. A technology that can accurately diagnose skin cancers could potentially impact the workload received by clinical laboratories and anatomic pathology groups.
—JP Schlingman
Related Information:
Dermatologists Hate Him! Meet the Skin-cancer Detecting Robot
Man Against Machine: Diagnostic Performance of a Deep Learning Convolutional Neural Network for Dermoscopic Melanoma Recognition in Comparison to 58 Dermatologists
AI Better than Dermatologists at Detecting Skin Cancer, Study Finds
AI May Be Better at Detecting Skin Cancer than Your Derm
Deep Learning Algorithm Does as Well as Dermatologists in Identifying Skin Cancer
Genomic Companies Collaborate to Develop Facial Analysis Technology Pathologists Might Eventually Use to Diagnose Rare Genetic Disorders