Aug 27, 2018 | Laboratory Management and Operations, Laboratory News, Laboratory Operations, Management & Operations, News From Dark Daily
Data generated by medical laboratories and diagnostic providers takes an increasing role in treatment and precision medicine and allows greater analysis of data and integration of data into the care process
Most anatomic pathologists recognize that the unstructured data that makes up most pathology reports also represents a barrier to more sophisticated use of the information in those pathology reports. One solution is for pathology groups to adopt synoptic reporting as a way to get a pathology report’s essential data into structured fields.
The healthcare marketplace recognizes the value of structured data. In 2012, venture capitalists funded a new company called Flatiron Health. Flatiron’s goal was to access the medical records of cancer patients specifically to extract the relevant—and generally unstructured—data and put it into a structured database. This structured database could then be used to support both research and clinical care for cancer patients.
How valuable is structured healthcare data? Just this February, Roche paid $1.9 billion to acquire Flatiron. At that point, Flatiron had assembled information about the health records of two million cancer patients.
But Roche (ROG.S), recognizing the value of data, was not done. In July, it entered into an agreement to pay $2.4 billion for the remaining shares of cancer-testing company Foundation Medicine that it did not own. Foundation Medicine sequences tumors and uses that genetic data to assist physicians in diagnosing cancer, making treatment decisions, and identifying cancer patients who qualify for specific clinical trials.
Anatomic pathologists play a central role in the diagnosis, treatment, and monitoring of cancer patients. It behooves the pathology profession to recognize that generating, storing, analyzing, and reporting the data generated from examinations of tumor biopsies is a critical success factor moving forward. Otherwise, other players and stakeholders will move past the pathology profession and stake their own claim to capturing, owning, and using that data to add value in patient care.
How Lack of Standards Impact Transfer of Patient Data
DATAMARK Inc., a business process outsourcing (BPO) company headquartered in El Paso, Texas, reports that analysts from Merrill Lynch, Gartner, and IBM estimate unstructured data comprises roughly 80% of the information in the average electronic medical record. This data could be the key to improving outcomes, tailoring precision medicine treatments, or early diagnosis of chronic diseases.
From narrative descriptions of biopsies to dictated entries surrounding preventative care appointments, these entries hold data that might have value but are difficult to collate, organize, or analyze using software or reporting tools.
To further complicate matters, each service provider in a patient’s chain of care might hold different standards or preferred methods for recording data.
“At this point, [standards] are not to a level that helps with the detailed clinical data that we need for the scientific questions we want to ask,” Nikhil Wagle, MD, Assistant Professor of Medicine, Dana-Farber Cancer Institute, Harvard Medical School, and Associate Member, Broad Institute, told the New York Times.
An oncologist at the Dana Farber Cancer Institute in Boston, Wagle and his colleagues are creating a database of metastatic breast cancer patients capable of linking medical records, treatments, and outcomes with their genetic backgrounds and the genetics of their tumors. Despite best efforts, they’ve only collected 450 records for 375 patients in 2.5 years.

Nikhil Wagle, MD (above), Assistant Professor of Medicine, Dana-Farber Cancer Institute, Harvard Medical School, and Associate Member, Broad Institute, is building databases that link patient outcomes and experiences with their EHRs. But sharing that information has proved problematic, he told the New York Times. “Patients are incredibly engaged and excited,” he said, “[But] right now there isn’t a good solution. Even though the patients are saying, ‘I have consented for you to obtain my medical records,’ there is no good way to get them.” (Photo copyright: Dana-Farber Cancer Institute.)
Additionally, once records are obtained, the information—sometimes spanning hundreds of faxed pages—must still be processed into data compatible with Dana-Farber’s database. And updating and maintaining the database requires a full-time staff of experts that must review the information and accurately enter it as required.
When critical concerns arise—such as a cancer diagnosis—information that could yield valuable clues about treatment options and improve outcomes might be held in any number of data silos in any number of formats.
This doesn’t account for the complexity of organizing such information for researchers who are developing new treatments, applying data to less targeted approaches, or dealing with privacy concerns between care providers.
Moving forward, those who can create and interact with data in a way that requires minimal human touch to make it suitable for analysis, further processing, or archiving, could communicate data more effectively and glean value from the growing trove of data silos created by laboratories around the world.
Big Pharma Making Big Bets on Structured Data
These are all the reasons why the recent moves by Roche show the importance and perceived value of structured medical records data as it takes an increasingly important role in precision medicine treatments and diagnosis.
With its acquisition of both Flatiron Health and Foundation Medicine, Roche has secured the ability to generate data, convert said data into a structured format to drive decisions, improve core data-related services, and promote the value of their offerings. This positions Roche to maximize the value of its data for internal use and marketing to researchers and other interested parties.
For clinical laboratories, pathology groups, and other diagnostics providers generating untold amounts of data daily, this highlights a critical opportunity to stay ahead of future trends and position themselves as valuable sources of information as healthcare data continues to play an essential role in modern healthcare.
—Jon Stone
Related Information:
New Cancer Treatments Lie Hidden under Mountains of Paperwork
Unstructured Data in Electronic Health Record Systems: Challenges and Solutions
Pharma Giant Roche Just Made a $2.4 Billion Bet on Cancer Data
Roche to Buy Flatiron Health for $1.9 Billion to Expand Cancer Care Portfolio
Why Drug Giant Roche’s $1.9 Billion Deal to Buy Data Startup Flatiron Health Matters
Roche Acquires the Outstanding Shares of Foundation Medicine for $2.4Bn
New Solutions for Unstructured Data May Help with Clinical Laboratory and Anatomic Pathology Data
Aug 24, 2018 | Instruments & Equipment, Laboratory Instruments & Laboratory Equipment, Laboratory Management and Operations, Laboratory News, Laboratory Operations, Laboratory Pathology, Laboratory Testing
CDC reports more than 93-million US adults are obese, and health issues related to obesity include heart disease, stroke, type 2 diabetes, and cancers
In recent years, the role of the human microbiome in weight loss or weight gain has been studied by different research groups. There is keen interest in this subject because of the high rates of obesity, and diagnostic companies know that development of a clinical laboratory test that could assess how an individual’s microbiome affects his/her weight would be a high-demand test.
This is true of a study published this year in Mayo Clinic Proceedings. Researchers at Mayo Clinic looked at obese patients who were in an active lifestyle intervention program designed to help them lose weight. It was determined that gut microbiota can have a role in both hindering weight loss and supporting weight loss.
Gut Microbiota More Complicated than Previously Thought
The Mayo researchers determined “an increased abundance of Phascolarctobacterium was associated with [successful weight loss]. In contrast, an increased abundance of Dialister and of genes encoding gut microbial carbohydrate-active enzymes was associated with failure to [lose] body weight. A gut microbiota with increased capability for carbohydrate metabolism appears to be associated with decreased weight loss in overweight and obese patients undergoing a lifestyle intervention program.”
How do bacteria impede weight loss? Vandana Nehra, MD, Mayo Clinic Gastroenterologist and co-senior author of the study, explained in a news release.
“Gut bacteria have the capacity to break down complex food particles, which provides us with additional energy. And this is normally is good for us,” she says. “However, for some individuals trying to lose weight, this process may become a hindrance.”
Put another away: people who more effectively metabolized carbohydrates were the ones who struggled to drop the pounds, New Atlas pointed out.

Vandana Nehra, MD (left), and Purna Kashyap, MBBS (right), are Mayo Clinic Gastroenterologists and co-senior authors of the Mayo study. “While we need to replicate these findings in a bigger study, we now have an important direction to pursue in terms of potentially providing more individualized strategies for people who struggle with obesity,” Nehra noted in the news release. Thus, precision medicine therapy for obese individuals could be based on Mayo Clinic’s research. (Photo copyright: Mayo Clinic.)
Mayo Study Provides Clues to Microbiota Potential in Weight Loss
The Mayo researchers wanted to know how gut bacteria behave in people who are trying to lose weight.
They recruited 26 people, ranging in age from 18 to 65, from the Mayo Clinic Obesity Treatment Research Program. Fecal stool samples, for researchers’ analysis, were collected from participants at the start of the three-month study period and at the end. The definition of successful weight loss was at least 5% of body weight.
Researchers found the following, according Live Science:
- 2 lbs. lost, on average, among all participants;
- Nine people were successful, losing an average of 17.4 lbs.;
- 17 people did not meet the goal, losing on average just 3.3 lbs.; and,
- More gut bacterial genes that break down carbohydrates were found in stool samples of the unsuccessful weight loss group, as compared to the successful dieters.
The researchers concluded that “An increased abundance of microbial genes encoding carbohydrate-active enzyme pathways and a decreased abundance of Phascolarctobacterium in the gut microbiota of obese and overweight individuals are associated with failure to lose at least 5% weight following a 3-month comprehensive lifestyle intervention program.”
Purna Kashyap, MBBS, Mayo Clinic Gastroenterologist and co-senior author of the study, told Live Science, “The study suggests there is a need to take the microbiome into account in clinical studies (on weight loss), and it also provides an important direction to pursue in terms of providing individualized care in obesity.” The very basis of precision medicine.
Future Weight-Loss Plans Based on Patient’s Microbiota
The Mayo Clinic researchers acknowledged the small sample size and need for more studies with larger samples over a longer time period. They also noted in their paper that Dialister has been associated with oral infections, such as gingivitis, and its role in energy expenditure and metabolism is unclear.
Still, the study suggests that it may soon be possible to give people individualized weight loss plans based on their gut bacteria. Clinical laboratory professionals and pathologists will want to stay abreast of follow-up studies and replication of findings by other research teams. A future medical laboratory test to analyze patients’ microbiomes could help obese people worldwide as well as lab business volume.
—Donna Marie Pocius
Related Information:
Gut Microbial Carbohydrate Metabolism Hinders Weight Loss in Overweight Adults Undergoing Lifestyle Intervention with a Volumetric Diet
Gut Microbiota from Twins Discordant for Obesity Modulate Metabolism in Mice
CDC: Adult Obesity Facts
Makeup of an Individual’s Gut Bacteria May Play Role in Weight Loss, Mayo Study Suggests
Struggle to Lose Weight? Your gut Bacteria May Be to Blame
Your Gut Bacteria May Make It Harder to Lose Weight
Diet Hit a Snag? Your Gut Bacteria May be Partly to Blame
Can’t Lose Weight? Your Gut Bacteria Could be to Blame, According to Study
Richness of Human Gut Microbiome Correlates with Metabolic Markers
Annual Medical Spending Attributable to Obesity: Payer- and Service-Specific Estimates
5 Ways Gut Bacteria Affect Your Health
Cornell Researchers Identify Gut Microbes That May Help Some People Remain Thin; Findings Could Result in Clinical Laboratory Tests to Analyze Microbiomes of Individuals
Clinical Laboratories Might Soon be Diagnosing Obesity and Guiding Therapies that Utilize Engineered Microbes
Aug 23, 2018 | Digital Pathology, Laboratory Management and Operations, Laboratory News, Laboratory Operations, Laboratory Pathology, Laboratory Testing, Management & Operations
Genetic testing, gene sequencing done by clinical laboratories and anatomic pathology groups underpin how first-mover hospitals, health networks are improving patient outcomes
In just a few weeks, an unprecedented gathering will bring together the nation’s most prominent first-mover health networks, hospitals, and companies operating programs that deliver precision medicine daily to patients in clinical care settings.
On Sept. 12-13, 2018, “Breakthroughs with Genetic and Precision Medicine: What All Health Network CEOs Need to Know,” will take place at the Hutton Hotel in Nashville, Tenn. “What differentiates these sessions is the emphasis on each organization’s strategy, how it launched its precision medicine programs, what is improving in patient outcomes, and how payers are reimbursing for these services,” stated Robert L. Michel, Executive Director of the Precision Medicine Institute in Austin, Texas. “This is not about the science of precision medicine. Rather, it is about the practical elements required for any hospital, health system, or physician group to actually set up and deliver a precision medicine service to patients on a daily basis.”
Precision Medicine’s First-Mover Hospitals and Providers to Speak
Health systems and hospitals headlining this special conference are:
Companies scheduled to present include:
- Illumina;
- Humana;
- Sonic Healthcare USA;
- Genome Medical;
- CQuentia, and,
- S. HealthTek.
Exhibitors include the above, plus: Thermo Fisher, Philips, Sunquest, and MyGenetx.
“This meeting will give you the insider’s understanding about delivering precision medicine in real patient care settings that cannot be accessed at other venues,” noted Michel. “The goal is to have first-mover providers share their experiences, thus providing a road map that other hospitals, physician practices, and other providers at this conference can take back and follow with confidence.”
Michel said that sessions will be dedicated to precision medicine strategies, how it is being used in oncology, primary care, the role of pharmacogenomics, and use of healthcare big data. Speakers will describe the clever ways innovative health networks and hospitals are using healthcare big data to inform physicians in ways that improve outcomes, lower the cost of care and, in two real-world case studies, are generating seven-figure reimbursement from shared savings programs with certain health plans.

This year’s keynote address is by Jeffrey R. Balser, MD, PhD (above), President and CEO, Vanderbilt University Medical Center and Dean of the Vanderbilt University School of Medicine, one of the most progressive and innovative health systems in the country. (Photo copyright: Vanderbilt University.)
Using Healthcare Big Data to Achieve Precision Medicine Success, Shared Savings
“Shared savings successes will be one of the breakthrough achievements reported at the Nashville event,” he explained. “We’ve invited two prominent provider organizations to share how they are using healthcare big data to support physicians in achieving improved patient outcomes while at the same time impressively reducing the overall cost of care. To my knowledge, this is the first time these precision medicine case studies have been presented at a national meeting.”
One such presentation will be delivered by Philip Chen, MD, PhD, Chief Healthcare Informatics Officer at Sonic Healthcare USA Austin, Texas. Their precision medicine goal was to use healthcare big data to help physicians better manage diabetes and other chronic conditions in their practices. This program involved a large primary care practice and a major health insurer. Now in its fourth year, Sonic Healthcare USA is earning six- and seven-figure payments as part of a shared savings arrangement with the insurer.
“Shared savings is definitely a Holy Grail for all large health networks and physician groups as payers drop fee-for-service and switch providers to value-based payments,” said Michel. “The experience of Sonic Healthcare in this innovative three-way collaboration with an insurer and a very large physician group demonstrates that a strong data analytics capability and engagement with physicians can simultaneously bend the cost-of-care-curve downward while improving patient outcomes, as measured year-by-year. This is a presentation every C-Suite executive should attend.
Strategic, Business, Operational, and Financial Aspects of Precision Medicine
“This conference—centered upon the strategic, business, operational, and financial aspects of a precision medicine program—came to be because it is the unmet need of every health network CEO and C-Suite administrator,” observed Michel. “Every healthcare leader tasked with developing an effective clinical and financial strategy for his or her institution knows that the real challenge in launching a precision medicine program for patient care is not the science.
“Rather, the true challenges come from how to support clinical needs with the availability of capital, recruiting experienced clinicians, and putting the right informatics capabilities in place,” he stated. “Most hospital and health network administrators recognize the risk of launching a precision medicine program too early. They know such programs can suck up huge amounts of resources without producing significant improvements in patient care. What adds to the risk is that payers may be slow to reimburse for precision medicine.”
Register today to guarantee your place at “Breakthroughs with Genetic and Precision Medicine: What All Health Network CEOs Need to Know,” (or copy and paste this URL in your browser: https://dark.regfox.com/precision-medicine-institute).
Register by September 1 and save $300 on tuition! Plus, take advantage of our special Team Discount Program, so you and your key team members can get the most out of the conference by attending together.
“Breakthroughs with Genetic and Precision Medicine: What All Health Network CEOs Need to Know” is the gold-standard summit for everyone active or interested in succeeding with precision medicine programs. Don’t miss out—register today!
—Michael McBride
Related Information:
Breakthroughs with Genetic and Precision Medicine: What All Health Network CEOs Need to Know—Full Agenda and Details
Breakthroughs with Genetic and Precision Medicine: What All Health Network CEOs Need to Know—Registration information
Ongoing Growth in Consumer Genetic Testing Pressures Hospitals, Healthcare Networks to Educate and Prepare Physicians
Syapse Creates Precision Medicine Council That Quickly Attracted 200 of the Biggest Hospitals and Health Networks as Members
When Ramping Up Genomic Programs, Health Network/Hospital CEOs and Executives Must Consider Emerging Technologies, Swiftly Rising Consumer Demand
Precision Medicine Success Hinges on Diagnostics’ Clinical Utility
Precision Medicine and Sharing Medical Data in Real Time: Opportunities and Barriers
Ongoing Growth in Volume of Clinical Laboratory Tests That Support Precision Medicine Due to Physician Acceptance; Payers Still Have Concerns
Aug 22, 2018 | Laboratory News, Laboratory Operations, Laboratory Pathology, Laboratory Testing, Management & Operations
Clinical laboratories should prepare to receive test orders from these mini-medical centers, based on consumer demand for quick, inexpensive, local healthcare
Is the era of clinical laboratory testing offered in retail stores soon to arrive? Dark Daily as long as 10 years ago predicted that walk-in clinics featuring a nurse or nurse practitioner who could diagnose and prescribe for a limited number of health conditions—which had a remedy that could be purchased at the pharmacy in the retail store—would be the door-openers to locating more sophisticated clinical services in retail settings.
Since then, we’ve covered many such openings—including free standing urgent care clinics opening in urban settings to service the consumer demands of busy patients—which have impacted clinical laboratories and anatomic pathology groups in predictable ways.
Late last year, UnitedHealth Group’s MedExpress and Walgreens Boots Alliance (NASDAQ:WBA] announced a joint pilot program to open urgent care centers attached to Walgreens stores.
The premise of the collaboration was based around the belief that consumers would welcome the opportunity and benefits of receiving basic healthcare services in a facility located next to a pharmacy. The Walgreens/MedExpress agreement, however, also indicates that two of the largest healthcare organizations in the world believe consumers would also be interested in visiting physicians who provided more sophisticated medical services, including critical care, in retail settings.
To date, Walgreens has opened MedExpress clinics in 15 locations in six states, including: Minnesota, Nebraska, Nevada, Texas, Virginia, and West Virginia. More such clinics are expected to open this year as part of the collaboration.

“MedExpress is a resource for busy families and employers that need timely access to affordable, high-quality healthcare close to home and work,” Fred Hinz (above), VP of Operations at MedExpress told Drug Store News. “Being connected to Walgreens will enable our patients to receive quality care and purchase any other items they need, all in one trip.” It also will likely result in increased orders for clinical laboratory testing from retail locations. (Photo copyright: Grand Island Independent.)
Future Health System Delivers Critical Care from Retail Locations
Motivated by consumer demand for convenient, high-quality healthcare, the urgent care market in the United States continues to grow. This trend will eventually influence clinical laboratories and anatomic pathology groups seeking to service these providers. It will be a dynamic market as new participants and mergers compete for leverage in this profitable business.
“This is just part of developing an overall higher-performing local health system,” Forbes reported UnitedHealth CEO David Wichmann telling analysts during the company’s earning call last month. “It’d just be one component that may be nested inside a local care delivery market with ambulatory surgical capacities and house calls and things of that nature. This is the future health system that we see delivering considerable value to people.”
The speedy growth in the number of and profitability of urgent care centers is another confirmation that this healthcare trend has legs. And experts believe the growth will continue and accelerate.
A recent report by market research and consulting firm MarketsandMarkets (MnM) predicts the global urgent care market should reach $25.93 billion (US) by the year 2023. The current value of the industry is $20 billion. The growth rate for the industry is expected to be 5.3% with North America being the region accounting for the highest amount of that growth.
The MnM report attributes the rise in the urgent care market to many factors, including:
- Growing investments in urgent care;
- Strategic developments between urgent care providers and hospitals;
- Access to affordable care;
- Convenience of shorter wait times; and,
- Increase in the geriatric population.
The report projects that the biggest hurdle facing the urgent care industry will be the lack of a skilled workforce.
Urgent Care a Growth Industry According to Experts
There are currently more than 7,500 urgent care facilities in the United States, according to an Urgent Care Association (UCA) white paper.
According to the UCA, the top six urgent care organizations in the US each have more than 100 locations. Those companies include:
A 2017 UCA benchmarking report states that only 3% of patients who are seen at an urgent care facility were diverted to an emergency room in 2016. The top diagnosis codes for visits during that year were:
- Acute upper respiratory infection;
- Unspecified acute sinusitis;
- Acute pharyngitis;
- Cough; and,
- Fever.
A report by Becker’s Hospital Review states that urgent care visits account for 19% of all healthcare visits in the US.
Urgent Care Centers Badly Needed and Highly Profitable
Last year, strategy consulting firm Health Systems Advisors (HSA) commissioned a study regarding the current and future need for urgent care centers. According to Becker’s Hospital Review, the HSA study stated that:
- “With the recent rise of urgent care development, there is an estimated 22% unmet need for urgent care in markets where urgent care sites could be financially viable;
- “The unmet demand is so large that approximately 1,600 new urgent care sites can be supported generating nearly $3.5 billion in revenue; and,
- “For health systems seeking to grow, the urgent care channel presents a unique opportunity to grow their revenue, influence patients’ downstream choices, and create a better experience for individuals desiring more convenience and better access.”
And data collected by FAIR Health indicates that, between 2007 and 2016, insurance claims for urgent care visits grew by a whopping 1,725%! Claims for emergency room visits increased by 229% during the same time period. FAIR Health is a non-profit organization that examines insurance claims for medical services for the purpose of bringing transparency to healthcare costs and insurance information.
Opportunities for Clinical Laboratories to Support Physicians
Clinical laboratories and pathology groups should pay attention to the burgeoning trend in urgent care, as those facilities order medical tests that will require processing, reading, and analyzing.
Exploring opportunities to serve urgent care centers offers clinical laboratories potential revenue streams and opportunities to serve the physicians practices and medical communities they support.
—JP Schlingman
Related Information:
UnitedHealth, Walgreens Partner to Put Urgent Care Next to Pharmacies
Report: MedExpress, Walgreens Pilots Grow to 15 Locations
Urgent Care Center Market by Service (Acute Illness Treatment, Trauma/Injury Treatment, Physical Examination, Immunization and Vaccination), Ownership (Corporate Owned, Physician Owned, Hospital Owned), and Region
Urgent Care Center Market on Track to Hit $26B by 2023
Urgent Care Industry Hits $18 Billion as Big Players Drive Growth
Health System Growth Using Urgent Care
20 Things to Know About Urgent Care
Top Urgent Care Organizations by Number of Centers
The Essential Role of the Urgent Care Center in Population Health
Patient Expectations Driving Growth in On-Demand Care
Urgent Care Centers: US Market Research Report
Consumer Trend to Use Walk-In and Urgent Care Clinics Instead of Traditional Primary Care Offices Could Impact Clinical Laboratory Test Ordering/Revenue
Aug 20, 2018 | Instruments & Equipment, Laboratory Instruments & Laboratory Equipment, Laboratory Management and Operations, Laboratory News, Laboratory Operations, Laboratory Pathology, Laboratory Testing, Management & Operations
“On-a-chip” devices continue to advance and medical laboratories will be natural repositories for patient data as the technology continues to improve
Dark Daily has predicted that the future of clinical laboratory testing will include highly complex multi-analyte test panels. The biomarkers, however, could number in the hundreds or thousands. So, it’s interesting to see new research by a Massachusetts Institute of Technology (MIT) team currently developing a multi-biomarker organ test device for clinical purposes.
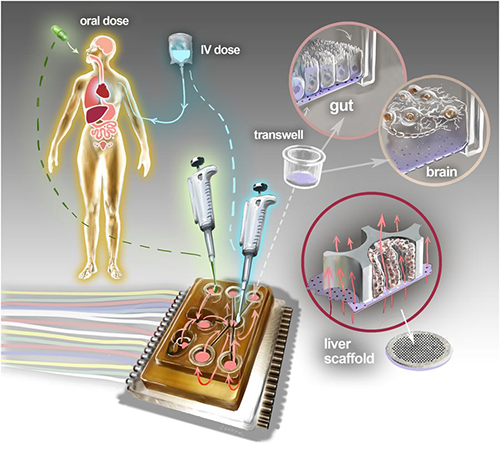
Motivated by the costly failure of animal testing efforts to develop drug safety and efficacy in humans, the MIT research engineers created a microfluidic platform technology they dubbed “physiome-on-a-chip,” or more colloquially, “body-on-a-chip.” Their goal is to identify drug reaction in different cell groups within the body (in vivo).
They acknowledged contributions of in vitro microphysiological systems (MPSs), AKA “organ-on-a-chip” (OOC) systems. They note, however, in their paper published in Scientific Reports, that more complex systems that interconnect and receive data from multiple MPSs are needed due to increasing limitations arising from drugs’ “lack of efficacy” rather than toxicity.
“Here we describe the development and implementation of multi-MPS platforms, AKA physiome-on-a-chip, supporting four-way, seven-way, and 10-way MPS interactions for several weeks,” the MIT engineers wrote.
Though MIT’s new technology needs further research and development time, as well as clinical trials, this type of chip design and its ability to scale is a positive development and progress toward Dark Daily’s prediction. Once finalized, it could be adopted in medical laboratories for many types of diagnostic testing purposes.
Researchers Motivated to Improve Drug Efficacy
According to an MIT news release, “MIT engineers have developed new technology that could be used to evaluate new drugs and detect possible side effects before the drugs are tested in humans. Using a microfluidic platform that connects engineered tissues from up to 10 organs, the researchers can accurately replicate human organ interactions for weeks at a time, allowing them to measure the effects of drugs on different parts of the body.”
The “body-on-a-chip” technology, MIT says, is aimed at determining how drugs may affect one organ while also having side effects on others.
“Some of these effects are really hard to predict from animal models because the situations that lead to them are idiosyncratic. With our chip, you can distribute a drug and then look for the effects on other tissues and measure the exposure and how it is metabolized,” said Linda Griffith, PhD, Professor of Teaching Innovation at MIT’s School of Engineering, and a senior author of the study, in the news release.
According to MIT, factors affecting the effectiveness of pharmaceuticals may include:
- Genetics;
- Environment;
- Personal lifestyles; and,
- Interactions with other drugs.
TechCrunch called the study “unprecedented,” pointing to the platform’s connection of so many tissues and the technology’s ability to keep them stable for weeks.

“An advantage of our platform is that we can scale it up or down and accommodate a lot of different configurations,” Linda Griffith, PhD, MIT Professor, MIT School of Engineering, told Science Daily. “I think the field is going to go through a transition where we start to get more information out of a three-organ or four-organ system, and it will start to become cost-competitive because the information you’re getting is so much more valuable.” (Photo copyright: MacArthur Foundation.)
How “Body-on-a-Chip” Works
“Body-on-a-chip” is about the size of a tablet computer and links 10 organ types, including: liver, lung, gut, endometrium, brain, heart, pancreas, kidney, skin, and skeletal muscle.
Using microfluidic platform technology, the researchers placed one- to two-million cells from human tissue samples into the device and then pushed fluid through the chip to resemble blood flow, the Daily Mail reported, adding that MIT’s MPS platform design features:
- Compartments made from a plastic block;
- Passages for fluid to move (as a circulatory system does) between the compartments;
- A water reservoir to limit fluid evaporation; and,
- Ability to monitor flow of molecular exchanges and drug distribution.
Essentially, using the MIT device, a drug can be introduced to one organ, processed normally, and then passed to other organs for processing and use in other ways, TechCrunch summarized.
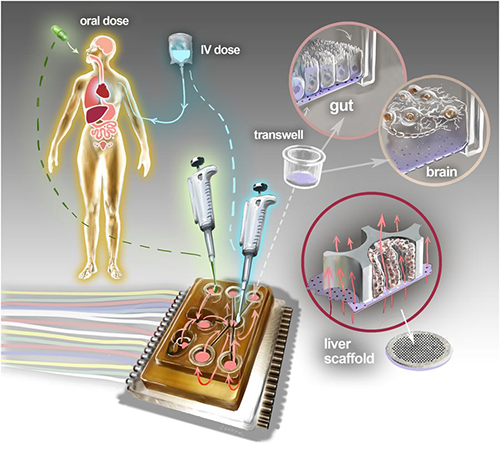
The physiome-on-a-chip system (above schematic) comprises bioengineered devices that nurture many interconnected 3D MPSs representing specified functional behaviors of each organ of interest, designed to capture essential features of in vivo physiology based on quantitative systems models tailored for individual applications such as drug fate or disease modeling. This technology could eventually be utilized for clinical laboratory and anatomic pathology testing. (Image and caption copyright: Victor O. Leshyk/Scientific Reports.)
Drug Delivery, Effects on Multiple Tissues Noted in MIT Study
The MIT researcher engineers reported these findings and accomplishments:
- Delivering a drug to the gastrointestinal tissue;
- Replicating digesting a drug;
- Observing as a drug was transported to other tissues and metabolized;
- Measuring a drug’s path; and,
- Noting effects of a drug on different tissues and how drugs break down.
“The huge potential of MPS technology is revealed by connecting multiple organ chips in an integrated system for in vitro pharmacology. This study beautifully illustrates that multi-MPS ‘physiome-on-a-chip’ approaches, which combine the genetic background of human cells with physiologically relevant tissue-to-media volumes, allow accurate prediction of drug pharmacokinetics and drug absorption, distribution, metabolism, and excretion,” said Kevin Healy, PhD, Professor of Bioengineering and Materials Science and Engineering, at University of California Berkeley in the MIT news release. Healy was not involved in the research.
Unique Device Design
In addition to making it possible to study so many different tissue types, the device design, according to MIT, is unique for these reasons:
- Its open microfluidic system, rather than a closed system, means the lid can be removed to manipulate tissue samples;
- Instead of external pumps common in closed systems, the MIT team used “on-board pumps” to control flow of liquid between the organs; and,
- The pumps used enabled larger engineered tissues, such as those from tumors in an organ, to be assessed.
The MIT engineers next plan to focus on specific organs—including the brain, liver, and gastrointestinal tissue—to model Parkinson’s disease, Digital Trends reported.
As healthcare providers and medical laboratories adopt precision medicine, MIT’s contributions are both timely and important. The ability to accommodate many different configurations in one platform is impressive, and something Dark Daily has been anticipating.
—Donna Marie Pocius
Related Information:
A “Body-on-a-Chip” Strings Together 10 Model Human Organs
“Body-on-a-Chip” Could Improve Drug Evaluation
MIT Builds “Body-on-a-Chip” Device That Can Store up to 10 Artificial Organs at Once
Interconnected Microphysiological Systems for Quantitative Biology and Pharmacology Studies
MIT Gadget Puts Multiple Artificial Organs into a Paperback-Sized Connected System
Drug Testing Could Get a Boost from MIT’s “Body-on-a-Chip”
Aug 17, 2018 | Digital Pathology, Laboratory News, Laboratory Operations, Laboratory Pathology, Laboratory Testing, Management & Operations
Pathologists might be able to help overburdened doctors by adding medical laboratory support services that assist providers in selecting the right tests and identifying the best therapeutic options for patients
In a new Stanford University School of Medicine study published in the July 9, 2018, issue of Mayo Clinic Proceedings, researchers indicate that physician burnout may be as big a cause of medical errors as unsafe healthcare environments. This highlights an opportunity for clinical laboratory professionals and pathologists to help physicians improve both diagnostic accuracy and the selection of the most appropriate therapies.
The study found that exhausted providers were twice as likely to report making a medical error. However, it’s a complex problem with no easy solutions.
“Just trying to fix the setting of healthcare environments in order to prevent errors is not sufficient,” Stanford University’s Daniel Tawfik, MD, MS, the study’s lead author, told Reuters Health. “We also need to address the actual underlying human factors that contribute to errors—specifically looking at physician burnout.”
Nevertheless, while there is no one-size-fits-all solution to physician burnout, clinical laboratory managers and pathologists potentially could help overburdened providers reduce burnout and fatigue by adopting new lab testing support services designed to assist physicians in selecting the right tests and identifying the best therapeutic options for their patients.
Medical Errors Third-Leading Cause of Death in America
Stanford researchers wanted to learn how physician burnout contributes to medical errors which, according to Johns Hopkins, is the third-leading cause of death in the US. They surveyed 6,695 physicians from across America. Of the respondents:
- More than 54% reported symptoms of burnout;
- 33% experienced excessive fatigue;
- Nearly 7% had thoughts of suicide; and,
- Roughly 4% reported a failing safety grade in their primary work area.
Even in medical units judged to have excellent safety records, the study found rates of medical errors nearly tripled when physicians working in those units had high levels of burnout. The prevalence of errors became similar to a non-burned-out physician working in a unit with a safety grade of “acceptable” or “poor.”
“We found that physicians with burnout had more than twice the odds of self-reported medical error, after adjusting for specialty, work hours, fatigue, and work unit safety rating,” Tawfik noted in a Stanford news release. “We also found that low safety grades in work units were associated with three to four times the odds of medical errors.”
According to the study, overall, 10.5% of physicians surveyed acknowledged in the prior three months making:
- An error in judgment;
- A wrong diagnosis;
- A technical mistake during a procedure;
- Prescribing a wrong drug/dosage; and/or,
- Ordering medication/intervention for the wrong patient.
While more than half of mistakes (55.4%) did not affect patient outcomes, or only caused a temporary problem (22.6%), more than 5% of errors did lead to major permanent health problems and 4.5% resulted in a patient death, the study found.
Radiologists, neurosurgeons, and emergency medicine specialists had the highest prevalence of error rates, with more than 21% of providers in each of those fields acknowledging recent mistakes.
Physicians reporting errors were more likely to have symptoms of overall burnout (77.6% versus 51.5%), as well as fatigue (46.6% versus 31.2%), than error-free providers. Physicians reporting recent errors also had a higher prevalence of suicidal thoughts (12.7% versus 5.8%), the study found.
Ted Hole, MD, a family practice physician in Ventura, Calif., is not surprised by the correlation between medical mistakes and overall well-being. “If your brain isn’t working right, you’re going to make errors,” Hole told the Ventura County Star. “That’s what burnout does. It makes your brain not work right.”
Stanford Connects Physician Burnout and Poor Workspace Safety Ratings
In their paper, the Stanford researchers argue a “combination of physician-targeted burnout interventions and unit-targeted patient improvement measures” are needed to tackle the problem of medical errors. Physicians who gave their work units an excellent, very good, or acceptable safety grade were less likely to make a medical error than those who described workplace safety as poor or failing.
Of the physicians who reported a poor or failing work unit safety grade, nearly 25% reported a recent error. Errors were incrementally lower for work units with higher safety grades regardless of physician burnout levels.
“This indicates both the burnout level as well as work unit safety characteristics are independently related to the risk of errors,” Tait Shanafelt, MD, Director of the Stanford WellMD Center and Associate Dean of the School of Medicine, noted in a Stanford statement.
“Today, most organizations invest substantial resources and have a system-level approach to improve safety on every work unit,” he said in the Stanford news release. “We need a holistic and systems-based approach to address the epidemic of burnout among healthcare providers if we are truly going to create the high-quality healthcare system we aspire to.”

Tait Shanafelt, MD (above), is Director of the Stanford WellMD Center, Associate Dean of the School of Medicine, and an author of the Stanford study. He maintains the “epidemic of burnout” among healthcare providers should receive as much attention as safety issues. Shanafelt became Stanford Medicine’s first Chief Wellness Officer in 2017. (Photo copyright: Stanford School of Medicine.)
Burnout Among Physicians Increasing
Other studies, including Medscape’s “Lifestyle Report 2017: Race and Ethnicity, Bias and Burnout,” confirm an upward trend in burnout rates among US physicians. In the Medscape study, 51% of physicians surveyed reporting being “burned out,” defined as a loss of enthusiasm for work, feelings of cynicism, and a low sense of personal accomplishment. Since the Medscape Lifestyle Report first queried physicians about burnout in 2013, the number of providers reporting burnout has increased 25%.
Physician burnout has been attributed to a variety of factors, including:
- Excessive workloads;
- Financial stress;
- Extra hours spent on clerical work or EHR-related tasks; and,
- Loss of human-to-human interaction between physician and patient.
Robert Lum, MD, an Oxnard, Calif.-based radiation oncologist, blames the shift to corporate-owned medical practices for some of the reported increases in burnout among physicians. Lum told the Ventura County Star he stays upbeat by never losing sight of why he became a physician.
“If you focus on the reason you went into medicine in the first place, which is to help people and marvel at the miracles modern medicine is able to do, then you’ll have less burnout,” he said.
Nevertheless, other solutions also can help. Clinical laboratories play a key role in maximizing physician/patient encounters. By extension, physicians and laboratories are linked in unique ways that enable labs to reduce physician burden and ensure positive healthcare outcomes.
—Andrea Downing Peck
Related Information:
Physician Burnout, Well-being, and Work Unit Safety Grades in Relationship to Reported Medical Errors
Study Suggests Medical Errors Now the Third Leading Cause of Death in the U.S.
Medical Errors May Stem more from Physician Burnout than Unsafe Health Care Settings
Study Says Rising Doctor Burnout Means Rising Medical Errors
In a First for U.S. Academic Medical Center, Stanford Medicine Hires Chief Physician Wellness Officer
Medscape Lifestyle Report 2017: Race and Ethnicity, Bias and Burnout
Physician Burnout a Key Driver of Medical Errors