Apr 2, 2018 | Digital Pathology, Laboratory Instruments & Laboratory Equipment, Laboratory Management and Operations, Laboratory News, Laboratory Operations, Laboratory Pathology, Laboratory Testing
Ever shrinking “lab-on-a-…” technologies, a boon to medical laboratories and anatomic pathologists in remote resource-strapped regions, also have a place in modern labs
Researchers took another leap forward in reducing the size of clinical laboratory diagnostic tests and observational tools. This demonstration involved lab-on-a-fiber technology and showed promise in both monitoring anatomic pathology biomarkers in vivo and supplementing the abilities of existing lab-on-a-chip and microfluidic devices.
Lab-on-a-Fiber Next Technological Step Toward Miniaturization
In 2013, Dark Daily reported on research into an implantable laboratory-on-a-chip (LOC) for monitoring blood chemistry during chemotherapy. It was a major breakthrough at the time, which promised new and powerful tools for cancer treatment regimens.
However, most LOC systems aren’t designed for wet environments. Also, while microfluidics and flexible membranes allow for smaller footprints and tighter placement, they are still invasive in ways that might make patients uncomfortable or make real-world use less than ideal. And, long-term use brings further complications, such as corrosion or foreign-body granulomas.
Thus, lab-on-a-fiber’s ability to function in vivo, is one of the device’s principal advantages, as ExtremeTech noted.
Lab-on-a-fiber technology addresses many concerns. It is small enough to insert directly into organs, muscle mass, or veins when used as biosensors. And the fibers can return a wealth of information by using light and reflection, while allowing for minimal discomfort and precision placement.
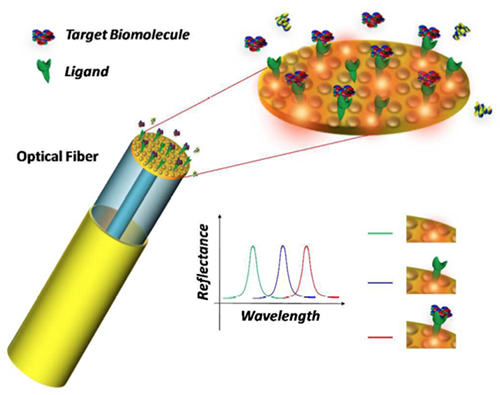
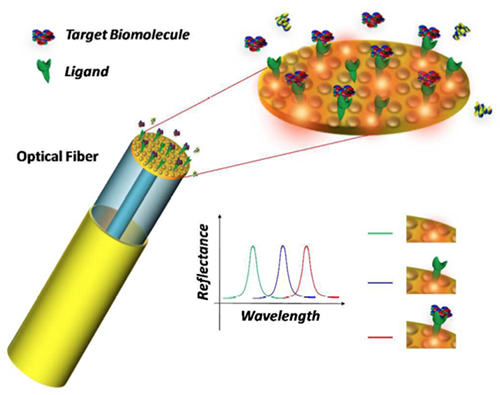
Schematic of the lab-on-a-fiber biosensing principle. A metallic nanostructure supporting a resonant plasmonic mode is integrated on the optical fiber tip. When a molecular binding event occurs at the sensor surface, the reflectance peak associated to the plasmonic mode shifts towards longer wavelengths. (Image and caption copyright: Analyst/The Royal Society of Chemistry.)
The Past and Future of Scaling Clinical Laboratory Testing
Dark Daily has followed these miniaturization trends for years starting with their earliest stages. A detailed timeline of developments can be viewed in “Lab-on-a-Chip Diagnostics: When Will Clinical Laboratories See the Revolution?” from 2016.
Additional Dark Daily “lab-on-a-…” coverage includes:
- IBM Watson Health and Mount Sinai Health System team up to use LOC solutions to separate biomolecules as small as 20nm from samples (See Dark Daily, “IBM and Mount Sinai Researchers Develop Innovative Medical Lab-on-a-Chip Solution,” October 3, 2016); and,
- Lab-on-Skin devices for monitoring biomarkers and electrophysiological signals, providing human-machine interfaces, and facilitating optogenetics (See Dark Daily, “In the Field of Nano-Scale Diagnostics, Many Researchers Are Developing ‘Lab-on-Skin’ Technologies That Can Monitor Many Clinical Laboratory Biomarkers,” January 15, 2015).
In the past year, a myriad of lab-on-a-fiber applications also have received media coverage, including:
Developers believe lab-on-a-fiber approaches could offer further adaptability and functionality to other “lab-on-a-…” technologies. For example, as highlighted in Advanced Science News, researchers are employing lab-on-a-fiber technologies to further refine and improve LOC functions and designs.
“As the scientific world moves inexorably to smaller dimensions … The emerging concept of ‘lab‐on‐fiber’ will give the optical fiber platform additional (highly integrated) functionalities,” noted Deepak Uttamchandani, PhD, Vice Dean Research, Faculty of Engineering, and, Robert Blue, PhD, Research Fellow, both at the University of Strathclyde, Glasgow, UK, in their review paper, “Recent Advances In Optical Fiber Devices for Microfluidics Integration.” The paper, published in the Journal of Biophotonics, examined “the recent emergence of miniaturized optical fiber-based sensing and actuating devices that have been successfully integrated into fluidic microchannels that are part of microfluidic and lab‐on‐chip systems.”

In his review paper on the emerging concept of lab-on-a-fiber, Deepak Uttamchandani, PhD, notes, “The versatility of the optical fiber platform has already allowed researchers to conduct immunoassays in microchannels using both fluorescently‐labelled and label‐free formats whilst gaining advantages of reduced assay time and increased sensitivity.” (Photo copyright: University of Strathclyde.)
Lab-on-a-Fiber: Another Step Forward or a Major Change?
At each milestone in the scaling of clinical laboratory testing, experts and media outlets predicted the demise of big laboratories and the dawn of a POC-centric testing era. Yet, despite 20-plus years of progress, this has yet to happen.
While it is critical for anatomical pathology leaders and clinical laboratory managers to stay abreast of developments in testing technology, much of the innovation behind lab-on-a-fiber remains strictly in the research realm. Challenges to the commercialization of these new techniques include both physical factors, such as design and manufacture of ready-to-use tests, and regulatory concerns, including FDA clearances and payer approval of new assays and diagnostic procedures.
Until researchers and test manufacturers overcome these hurdles, threats to current standards and workflows are minimal. However, much like the gains in scale realized through incorporating lab-on-a-chip concepts into clinical laboratory testing, the research powering these innovations might prove useful in further improving and expanding medical laboratory testing options.
—Jon Stone
Related Information:
Optical Fiber Devices for Microfluidics Integration Open Up New Horizons for Advanced “Lab-on-a-Chip” Technologies
Recent Advances in Optical Fiber Devices for Microfluidics Integration
Lab-on-Fiber Technology: A New Vision for Chemical and Biological Sensing [Abstract]
Lab-on-Fiber Technology: A New Vision for Chemical and Biological Sensing [Full Downloadable PDF]
How We’re Shrinking Chemical Labs onto Optical Fibers
Lab-on-Fiber Could Shine Light on Disease
Doctors Might Soon Diagnose You by Feeding a Lab-on-a-Fiber Straight into Your Veins
Fiber-Optic Device Can Detect Stray Cancer Cells and Improve Tumor Removal: Study
Fiber Optic Probe Beats a Biopsy for Measuring Muscle Health
Lab-on-a-Chip Diagnostics: When Will Clinical Laboratories See the Revolution?
Implantable Medical Laboratory-on-a-Chip Continuously Monitors Key Chemicals in Chemotherapy and High-Risk Patients
In the Field of Nano-Scale Diagnostics, Many Researchers Are Developing ‘Lab-on-Skin’ Technologies That Can Monitor Many Clinical Laboratory Biomarkers
Hematology on a Chip: University of Southampton Develops POC Blood Analysis
Sleek ‘Lab in a Needle’ Is an All-in-One Device That Detects Liver Toxicity in Minutes during a Study, Showing Potential to Supplant Some Medical Laboratory Tests
Whole Animal Assays Use Lab-on-a-Chip at MIT
IBM and Mount Sinai Researchers Develop Innovative Medical Lab-on-a-Chip Solution
In the Field of Nano-Scale Diagnostics, Many Researchers Are Developing ‘Lab-on-Skin’ Technologies That Can Monitor Many Clinical Laboratory Biomarkers
Mar 30, 2018 | Compliance, Legal, and Malpractice, Digital Pathology, Instruments & Equipment, Laboratory Management and Operations, Laboratory News, Laboratory Operations, Laboratory Pathology, Laboratory Testing, Management & Operations
Developers believe participants will be interested in controlling how their private health data is provided to medical laboratories, drug companies, research organizations, and the federal government, while also earning an income
Bitcoins for blood tests, anyone? A new venture is examining the idea of exchanging cryptocurrency, a digital asset, for the results of weekly clinical laboratory tests and photographs of body parts from healthcare consumers. If successful, in a couple of years, people might be able to earn a “basic income” from selling their private health data to pharmaceutical companies, medical laboratories, research organizations, the federal government, and more.
Insilico Medicine, a Baltimore developer of artificial intelligence (AI) solutions for research and pharmaceutical companies, and the Bitfury Group, a blockchain technology company based in Amsterdam, Holland, are working together on the project they call Longenesis, a blockchain-based platform that uses AI to collect, store, manage, and trade data, such as medical records and health data.
Marketing Human Life Data
The two participants presented their novel idea this past November in Taipei, Taiwan, at the TaiwanChain Blockchain Summit. They published their report in Oncotarget, an open-access biomedical journal that covers oncology research. The authors of the paper believe blockchain and AI technologies could support patients and physicians in working with medical data.
“There are many companies engaged in the marketplaces of human life data with billions of dollars in turnover. However, the advances in AI and blockchain allow returning the control of this data back to the individual and make this data useful in the many new ways,” Alex Zhavoronkov, PhD, founder of Insilico Medicine, told Cryptovest.
“I would love to live in a world where I’m motivated to regularly take all kinds of medical tests for free, I get the data back, and I will be able to sell this data to the marketplace, and I earn all kinds of goods and services—primarily health related,” Zhavoronkov told Motherboard.

Alexander Zhavoronkov, PhD, Founder and CEO of Insilico Medicine, told Motherboard, “Right now, it’s difficult to predict. But I think that if [users] submit blood tests, pictures, transcriptomes let’s say on a weekly basis, you probably will be able to earn a good universal basic income.” Zhavoronkov is describing a new business model involving clinical laboratory testing. (Photo copyright: Insilico Medicine.)
Combining blockchain and AI technologies is one of the many emerging technological advances emerging to enhance the medical and pharmaceutical industries.
“Recent advances in machine intelligence turned almost every data into health data. The many data types can now be combined in the new ways: one data type can be inferred from another data type and systems learning to optimize the lifestyle for the desired health trajectory can now be developed using the very basic and abundant data,” noted Polina Mamoshina, research scientist at Pharma AI, a division of Insilico Medicine, during the company’s presentation at TaiwanChain. “Pollen, weather, and other data about the environment can now be combined with the human biomarkers to uncover and minimize the allergic response among the myriad of examples. People should be able to take control over this data.”
Because pharmaceutical companies rely on data mining to obtain individual demographic information and medical records, the growth potential for this type of product is huge.
Clinical Laboratory Test Results Earn LifePound Tokens
Longenesis is still being tested, but Zhavoronkov hopes it will be ready for the public within the next two years. The plan is to utilize blockchain technology to collect and store patient medical data in exchange for their cryptocurrency, known as LifePound.
According to the Longenesis website, “Longenesis is a marketplace, which uses personal health data, transformed into a LifePound token. LifePound is used inside a marketplace as a monetary system, powered by Exonum blockchain technology to keep data secure and transparent. Tokens are distributed between Longenesis marketplace members and are used for transactions between the following elements:
- Developers;
- Users;
- Data providers;
- Customers; and the,
- Stock cryptocurrency market.
The developers believe the “Longenesis Data Marketplace will be able to provide new insights in the fields of healthcare research and development. It will provide analysis and recommendations to pharmaceutical companies to help develop new drugs.”
It’s too early to predict whether Longenesis will be successful and catch on with the public. However, the popularity of cryptocurrency, and the opportunity to earn an income from one’s clinical laboratory data, could encourage individuals to participate in this type of endeavor.
In addition, this is a highly unusual and unexpected approach to encourage consumers to undergo regular medical laboratory testing in order to earn payment by a digital currency. It is a reminder of how rapid advances in a myriad of technologies are going to make it possible for entrepreneurs to create new business models that involve clinical laboratory tests and the data produced by such tests.
—JP Schlingman
Related Information:
This Biotech Company Wants You to Give It Selfies and Blood Tests in Exchange for Cryptocurrency
A Decentralized Medical Record Marketplace Powered by Human Data
Blockchain, AI Could Spur Biomedical Research, Insilico Medicine Says
Converging Blockchain and Next-generation Artificial Intelligence Technologies to Decentralize and Accelerate Biomedical Research and Healthcare
Blockchain, Explained
Mar 28, 2018 | Laboratory Hiring & Human Resources, Laboratory Instruments & Laboratory Equipment, Laboratory Management and Operations, Laboratory News, Laboratory Operations, Laboratory Pathology, Laboratory Testing, Management & Operations
Microhospitals already offer most of the critical features of traditional hospitals, and by featuring telemedicine technology at the point of care, they are becoming powerful tools for healthcare providers
Dark Daily reported in January that microhospitals are opening nationwide, including in such innovative states as Texas, Colorado, Nevada, and Arizona. In addition to being open 24/7 and mostly located in high-density areas, these scaled down hospitals feature the most critical aspects of full-size hospitals—medical laboratories, emergency departments, pharmacies, and imaging centers.
However, a report by the Health Resources and Service Administration (HRSA) predicted that by 2020 the US will be short as many as 20,000 primary care physicians! Many specialty practices also are expected to see stiff shortages of physicians in the near future. Without enough physicians, even microhospitals cannot provide adequate care.
Thus, the ever increasing practice of using telemedicine as a way to serve more people, while providing faster, more efficient care tailored to meet the needs of individuals and communities, is welcomed news. If this trend becomes more widespread, it will create new opportunities and challenges for clinical laboratories in hospitals, as well as health systems that own and operate microhospitals.
Filling a Need in Vulnerable Communities
At the end of 2016, there were approximately 50 microhospitals operating in the United States, mostly in the Midwest, Arizona, Colorado, Nevada, and Texas. Sometimes referred to as neighborhood or community hospitals, microhospitals are acute care facilities that are smaller than traditional hospitals but can deliver many of the same medical services. They provide more comprehensive treatments than typical urgent care and outpatient centers and fill a gap between freestanding healthcare centers and major hospitals.
Microhospitals typically have less than a dozen short-stay beds and have the ability to provide inpatient care, emergency care, and imaging and medical laboratory services. And, they are usually affiliated with larger healthcare systems, which allows them to expand into certain areas without incurring the high costs of building a full-scale hospital.
“Right now they seem to be popping up in large urban and suburban metro areas,” Priya Bathija, Vice President, Value Initiative American Hospital Association, told NPR. “We really think they have the potential to help in vulnerable communities that have a lack of access.”
Patient Satisfaction and Declining Physician Populations Drive Demand for Telemedicine
Telemedicine, a combination of telecommunications and information technology, is primarily used to remotely connect healthcare providers to patients during office visits. But it also is being used successfully at the point of care in emergency departments and even surgery.
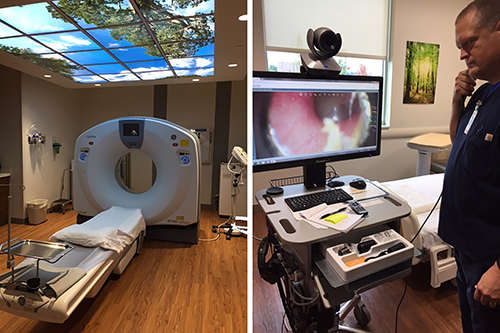
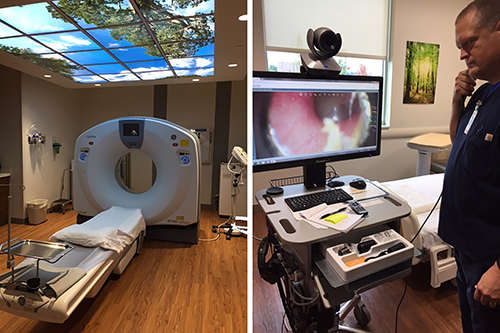
Microhospitals like St. Vincent Neighborhood hospital in Noblesville, Ind., which offer most of the critical functions of traditional hospitals, such as clinical laboratories, ERs, and the CT scanning station above (left), are increasingly including telemedicine technologies (above right) at the point of care to offset reductions in primary care and specialty physicians. (Photo copyright: Jill Sheridan/IPB News.)
Consumers are becoming more accepting of telemedicine (AKA, telehealth) as these services offer savings in both time and money. A recent survey by the Health Industry Distributors Association (HIDA) found that many patients were pleased with telehealth services. More than 50% of the surveyed individuals stated they were very satisfied with a recent telemedicine encounter. In addition, 54% of those individuals described their telehealth experience as better than a traditional, in-person office visit.
Telemedicine and Microhospitals Mutually Beneficial, According to HRSA
Other research suggests microhospitals may generate a mutually beneficial alliance with telemedicine that increases the progress of both entities, especially when considering projected increases in the number of nurse practitioners and physician assistants.
In its report, “Projecting the Supply and Demand for Primary Care Practitioners Through 2020,” Health Resources and Service Administration (HRSA) estimates there will be a shortage of more than 20,000 primary care physicians working in the US by the year 2020. Other specialties expected to experience staff shortfalls include:
Anticipation of this decline in physician numbers is fueling the demand for telemedicine to help with patient loads, especially in remote areas.
Saving Time and Money with Televisits
A study by Nemours Children’s Health System indicates that telemedicine may reduce medical costs for both patients and healthcare providers while sustaining patient satisfaction.
“At Nemours, we’ve seen how telemedicine can positively impact patients’ lives,” Shayan Vyas, MD, Medical Director of Telehealth at Nemours, noted in a press release. “The overwhelmingly positive response we’ve seen from parents who are early adopters of telemedicine really reinforces the feasibility of online doctor visits and sets the stage for real change in the way healthcare is delivered.”
The Nemours study involved 120 patients under the age of 18. The majority of families surveyed stated they would be interested in future telehealth visits and an impressive 99% said they would recommend telemedicine to other families.
The study discovered that patients and family members saved an average of $50 and about an hour of time, by utilizing telehealth for sports medicine appointments. The health system also experienced some monetary perks with the televisits, as they cost approximately $24 less per patient.
“We know that telemedicine is often looked to for common childhood ailments, like cold and flu, or skin rashes. But we wanted to look at how telemedicine could benefit patients within a particular specialty such as sports medicine,” Alfred Atanda Jr, MD, Pediatric Orthopedic Surgeon at Nemours/Alfred I. DuPont Hospital for Children in Wilmington, DE., told FierceHealthcare. “As the healthcare landscape continues to evolve and the emphasis on value and satisfaction continues to grow, telemedicine may be utilized by providers as a mechanism to keep costs and resource utilization low, and to comply with payer requirements.”
Healthcare consumers and providers are increasing looking to technology to enhance medical care and solve resource shortfalls. Separately, telehealth and microhospitals already help with these needs, Combined, however, they are a powerful solution to our nation’s reducing ranks of primary care physicians and medical specialists.
If this trend of microhospitals using telemedicine should continue and increase, both components will give medical professionals vital tools to provide faster, more economical, and more personalized services, to more patients across wider areas of America.
—JP Schlingman
Related Information:
Why Telehealth is Fueling the Move Towards Microhospitals
Projecting the Supply and Demand for Primary Care Practitioners Through 2020
Are Microhospitals the Answer for Systems Looking for Low-cost Expansions? They Might Be
Microhospitals: Healthcare’s Newest Patient Access Point
Microhospitals Could Prove Financial Boon and Salvation to Healthcare Systems
Microhospitals Provide Health Care Closer to Home
Telemedicine Saves Patients Time and Money, Study Shows
5 Common Questions about Micro-Hospitals, Answered
Survey: More than Half of Patients Prefer Telehealth Visits to In-Person Care
Majority of Parents Plan to Use Telemedicine for Pediatric Care
Microhospitals May Help Deliver Care in Underserved Areas
“Thinking Small” May Be Next Big Innovation in Healthcare Delivery as Microhospitals Spring Up in Metropolitan Areas Across Multiple States
Mar 26, 2018 | Compliance, Legal, and Malpractice, Laboratory Management and Operations, Laboratory Operations, Laboratory Pathology, Laboratory Testing, Management & Operations, News From Dark Daily
As the public gains awareness of the role clinical laboratories play in modern healthcare, increased engagement and understanding of the technology underlying many of these advances could create risk for labs without transparent reporting protocols to both patients and the public
In recent years, consumers have continually raised the bar in their expectation of quality when they interact with the healthcare system. Not only do patients expect providers—including clinical laboratories and anatomic pathology groups—to improve regularly over time, but the public has even less tolerance for medical errors of any type. Thus, a recent NPR story is one more warning to the medical laboratory profession that it should be devoting resources and effort to improving quality.
Today’s healthcare consumers and patients are more educated about and involved in the care process than ever before. While the exact science and skills may not interest the general public, the technologies underpinning much of the shift toward personalized medicine (AKA, precision medicine) are the same technologies that created the always-connected, digital lifestyles seen around the world.
With this, comes a level of scrutiny and questioning from the public that clinical laboratories or anatomic pathology groups would not have experienced even just a decade ago.
Mounting Scrutiny of Medical Laboratories and Healthcare Professionals
A recent segment on NPR’s “All Things Considered” highlighted this trend and questioned the quality control standards behind many of the procedures powering current testing. The segment also questioned the impact quality control has on the quality of biobanks used to research and create future technologies and tests.
Pathologist Richard Friedberg, PhD, Medical Director of Baystate Reference Laboratories and former president of the College of American Pathologists, told NPR, “We need to be sure that the stuff [doctors and researchers are] looking at is valid, accurate, reliable, and reproducible … If it’s garbage in, it’s garbage out.”
The story highlights improved standards and guidelines surrounding immunohistochemical (IHC) HER2 tests in the early 2000s. In 2007, The New York Times questioned the reliability of the tests, based on studies presented to the American Society of Clinical Oncology the week prior.
In response, the American Society of Clinical Oncology and the College of American Pathologists released guideline recommendations outlining the exact standards required to reduce assay variation and ensure that data produced is accurate and reproducible. NPR’s coverage claims this is the only test with such strict guidelines.
“I don’t think physicians think this way about their entire medical system,” Carolyn Compton, PhD, CMO of the National Biomarker Development Alliance, CMO of the Complex Adaptive Systems Initiative, and professor of Life Sciences at Arizona State University, told NPR. “I don’t see how we’re going to get precision medicine at the end of the day when everything under the hood is so imprecise.”
When data and previous research powers much of the innovation taking place across the modern healthcare landscape, the accuracy of said data would seem critical. Yet, without standards in place, there’s not always safeties by which to verify sample integrity and other critical concerns.
Late last year, Dark Daily reported on a study published in PLOS ONE from Radboud University in the Netherlands questioning the accuracy of more than 30,000 published scientific studies that contained misidentified or contaminated cell lines. Guidelines, such as those created for IHR and FISH HER2 testing, provide standards intended to prevent such issues from occurring or detecting them when they do occur.
Quality versus Quantity: A Gamble Worth Taking?
Apart from challenges with healthcare reform and the regulatory landscape surrounding precision medicine, medical laboratories also must struggle with the challenges of gleaning and maintaining useful, accurate information from an ever-growing trove of data produced by analyzers and assays.
Yet, these mediocre datasets include the results of tests that carried a potentially significant impact on patient lives. In the first two weeks of February alone, both the St. Louis Post-Dispatch and The Telegraph published stories related to erroneous testing related to cancer and the potential impact on the clinical laboratories involved and the patients tested.
Increased coverage shows that the world is watching what goes on in medical laboratories, hospitals, and data centers as healthcare continues to evolve. Clinical laboratories must move forward with this in mind or risk pushback and questioning from the public. Transparency regarding standards, and reporting information to patients surrounding testing or concerns, might effectively address this rising trend.
“We are moving faster and faster and faster as this whole precision medicine train is moving down the track,” Tim Allen, MD, Laboratory Director at the University of Texas Medical Branch Department of Laboratory Services, told NPR. “I suspect standardization of these things is going to become a reality much quicker than I would have expected even a few years ago.”
That quality control issues in anatomic pathology are considered newsworthy by no less than NPR is a sign of increased public attention to the quality of lab testing. The story was written to educate the public about the gap that exists in the quality control of anatomic pathology testing. All of this is consistent with the trend for providers to be transparent and report their quality metrics to the public, including patients.
—Jon Stone
Related Information:
Hormone Receptor Testing Volume 1: Investigation and Findings Commission of Inquiry on Hormone Receptor Testing
Precision Medical Treatments Have a Quality Control Problem
HER2 TESTS: How Do We Choose?
Cancer Drug May Elude Many Women Who Need It
American Society of Clinical Oncology/College of American Pathologists Guideline Recommendations for Immunohistochemical Testing of Estrogen and Progesterone Receptors in Breast Cancer
Impact of Electronic Health Record Systems on Information Integrity: Quality and Safety Implications
His Doctor Said It Was Cancer. It Wasn’t. But the Lab Mix-Up News Came Too Late.
Up to 60,000 Cancer Test Results May Have to Be Reviewed After Women Wrongly Given the All-Clear
Over 30,000 Published Studies Could Be Wrong Due to Contaminated Cells
Netherlands University Researchers Question Validity of More Than 30,000 Published Scientific Studies; Findings Have Implications for Medical Laboratories
Mar 21, 2018 | Digital Pathology, Instruments & Equipment, Laboratory Instruments & Laboratory Equipment, Laboratory Management and Operations, Laboratory News, Laboratory Operations, Laboratory Pathology, Laboratory Sales and Marketing, Laboratory Testing, News From Dark Daily
January’s press release confirmed the tech company is working to integrate critical medical data into its mobile devices, while further promoting interoperability and patient access
While interoperability has improved since the earliest electronic health record (EHR) systems, today’s active patients often need to sort through multiple healthcare portals—including those of clinical laboratories and anatomic pathology groups—to get a comprehensive view of their medical history. Not only can this be time consuming, but also inconvenient if the patient lacks access to a computer.
Thus, it’s no surprise that in a January 24 press release, mobile technology giant Apple announced plans to enter the development ring and create an improved EHR for its mobile device users by updating its existing “Health” mobile application (app). The iOS 11.3 update, among other things, is designed to enable Apple iPhone owners to receive critical medical data, such as medical laboratory test results, directly on their devices.
“Our goal is to help consumers live a better day. We’ve worked closely with the health community to create an experience everyone has wanted for years—to view medical records easily and securely right on your iPhone,” said Apple COO Jeff Williams in the press release.
Jeff Williams (above), COO at Apple, notes that, “By empowering customers to see their overall health, we hope to help consumers better understand their health and help them lead healthier lives.” (Photo copyright: Apple.)
The new features are already available to developers in the latest iOS 11.3 beta 3 release. However, release to the public is expected soon with the issuance of the iOS 11.3 final release. This means that patients will not need to download extra apps—or remember to use them—to take advantage of the feature.
New Way to Improve Patients’ Access to Health Data or Just Another Data Silo?
The Apple Health Records platform adheres to Fast Healthcare Interoperability Resources (FHIR) protocols for transmission of data. Providers send information to Apple which then aggregates the information, transmits it to patients’ iPhones and notifies them of the updates.
All information stored on the device is encrypted in storage and protected from unauthorized access by the user’s password.
Through the new Health Records interface, users view this aggregated data as a timeline, conduct searches, and share information with other parties as they deem appropriate.
Current medical information listed in the press release includes:
- Allergies;
- Conditions;
- Immunizations;
- Clinical laboratory results;
- Medications;
- Procedures; and,
- Vitals.
Currently, the platform integrates data from three major EHR developers:
- Epic;
- Cerner; and,
- AthenaHealth

Apple’s update to the Health app makes it easier for people to access and control of all of their health records and data. This included medical laboratory tests. (Image and caption copyright: Apple.)
Apple is also working with 12 health institutions across the US in the first phase of the project, including:
In the Apple press release, Stephanie Reel, CIO at John Hopkins Medicine in Baltimore, stated, “Streamlining information sharing between patients and their caregivers can go a long way towards making the patient experience a positive one. This is why we are excited about working with Apple to make accessing secure medical records from an iPhone as simple for a patient as checking email.”
Previous Attempts at Mobile Health Record Devices Got Mixed Results
This isn’t the first time a major technology company has attempted to enter the mobile health market. Google Health was shuttered in 2011 citing low adoption. Wearable fitness trackers, such as Fitbit (NYSE:FIT) enjoyed a bubble, but are now seeing mixed success in terms of long-term adoption and use, according to The Motley Fool. More to the point, they’ve never quite become the holy grail of monitoring and data collection that some experts predicted, Huffington Post reported.
However, Apple’s investments and interest in healthcare-related technologies has led to wide speculation that they would enter the health market this year. (See Dark Daily “Apple May Be Developing Mobile Device Technology to Monitor User’s Health and Transmit Data in Real Time.”)
Larry Dignan, Editor-in-Chief at ZDNet, builds a compelling case for why this could be the attempt that succeeds in providing a consolidated platform for clinical laboratories, physicians, and other care providers to push data directly to patients and—with the patient’s permission—to each other, regardless of the platforms healthcare facilities use to store and transmit data.
He notes that much of Apple’s newest features build on foundations laid by the healthcare industry to create scalable, functional EHR systems. By working with existing protocols, Apple’s Health Records platform is already positioned for compatibility with many healthcare providers.
Furthermore, Apple is already known for partnering at the enterprise level with major businesses and industries, while also holding the trust of millions of Americans who store their personal information on Apple devices.
Is Apple the Future of EHRs?
Despite this, until the platform—and adoption by the public—is proven a success, it will be yet another walled garden of medical information. Even then, Apple is only one segment of the global mobile market.
Unless Apple provides access to other platforms (such as Android), those patients—and the medical communities serving them—are left consolidating information on their own through a sprawl of various portals. This also means that medical laboratories, pathology groups, and other service providers must continue to invest time and funding into communicating data in ways compatible with a plethora of internal and external systems and software.
Still, the platform offers an intriguing glimpse at the future of medical records and heralds a shift toward empowering patients with easy, comprehensive access to their own data, which would be a boon to the medical laboratory industry.
—Jon Stone
Related Information:
Apple Previews iOS 11.3
Apple Announces Effortless Solution Bringing Health Records to iPhone
With Medical Records Tools, Apple Wades Deeper into Digital Health
Apple Confirms “Health Records” Solution with Aim to Bring Medical Records to iPhone
Apple Will Let You Keep Your Medical Records on Your iPhone
Apple Unveils mHealth Integration with EMR Data through Health App
Apple, Inc. Wants to Solve the Problem of Electronic Health Records
Viewpoint: How Realistic Is Apple’s Attempt at the EHR Industry? Very—6 Reasons Why
Apple Can Win Electronic Medical Record Game with Health Records in iOS 11.3: Here’s 7 Reasons Why
Apple Is Officially in the EHR Business. Now What?
Apple to Launch Health Records App with HL7’s FHIR Specifications at 12 Hospitals
Could Amazon or Apple Actually Make a Dent in the EHR Market?
Apple May Be Developing Mobile Device Technology to Monitor User’s Health and Transmit Data in Real Time
Mar 19, 2018 | Compliance, Legal, and Malpractice, Laboratory Management and Operations, Laboratory News, Laboratory Operations, Laboratory Pathology, Laboratory Testing, Management & Operations
The Joint Commission’s recent alteration to the Introduction to Leadership (LD) Standard LD.04.03.09 makes it easier for off-site and independent reference laboratories to service CLIA-hospitals and other CLIA-approved healthcare facilities
Anatomic pathologists working for reference laboratories can now provide diagnostic services to hospitals, critical-access hospitals, and ambulatory care facilities in the US based on the organization’s Clinical Laboratory Improvement Amendments (CLIA) status, rather than the usual credentialing and privileging. The Joint Commission (TJC) made the change effective January 2018.
According to a TJC press release, “Clinical Laboratory Improvement Amendments (CLIA) regulations 42 CFR 493.1351 through 493.1495 outline specific and rigorous competency requirements for laboratory personnel, including requirements for pathology services and its subspecialties. But because pathologists practicing in the US are required to comply with these requirements, Joint Commission-accredited organizations that seek the services of pathologists within independent reference laboratories (that comply with CLIA regulations) can safely presume that the pathologists are qualified and competent to perform all diagnostic services within their pathology practice—thus making an additional credentialing and privileging process unnecessary.”
In an interview with Dark Daily, Heather Hurley, Executive Director, The Joint Commission, and Ron Quicho, Associate Project Director and Standards Development Director at TJC, explained the reasons behind this change. “With the current CLIA requirements, the previous standard was adding unnecessary burdens and regulatory overhead to hospitals and ambulatory care organizations—especially as outsourcing continues to increase within the testing market. This update helps to reduce these burdens and streamline testing,” Hurley noted.
Quicho added, “The Joint Commission continually evaluates its standards and survey process to ensure that we are providing an accreditation service that is of the highest quality and value. That said, we made the decision to update the standards based on feedback from stakeholders and customers.”

Ron Quicho, Associate Project Director and Standards Development Director (left), and Heather Hurley, Executive Director (right), The Joint Commission, believe these updated standards will benefit clinical laboratories and hospitals alike. But they note, “Anytime the pathologist provides professional services and consultation in the same laboratory where the specimen was collected or prepared, credentialing and privileging would be required. The exception for credentialing and privileging only applies when pathology services are provided off-site, such as at a reference laboratory.” (Photo copyrights: LinkedIn/The Joint Commission.)
Joint Commission Reduces ‘Unnecessary Burden’ on Hospitals, Ambulatory Care Facilities
Reference testing and CLIA have been a common part of the diagnostics and medical laboratory landscape for decades. According to Quicho, the key components of The Joint Commission’s decision include:
- Increasing numbers of independent practitioners and consultants;
- Reference laboratories often seek pathology services from another laboratory for certain testing and screening. As such, it is unclear if the credentialing and privileging requirements extend to these secondary pathology services, since they may also be providing the interpretation;
- It would be virtually impossible to credential and privilege all pathologists at a reference laboratory whose services result in patient care decisions, since interpretations are made not only in anatomical (surgical) pathology but in many areas of clinical pathology; and,
- Reference laboratories employ hundreds of pathologists and healthcare facilities and cannot be sure of who provides interpretation on specimens that are sent out.
It is important to understand that the exclusions in this latest TJC update only apply when testing is performed offsite of the ordering facility. In their press release, TJC stated, “A reference laboratory is a laboratory contracted for testing that is owned and operated by an organization other than the organization referring the testing … When the pathologist provides his or her professional service, including consultation in the same laboratory or organization where the specimen was collected or prepared, credentialing and privileging is required.”
TJC Change Helps Clinical Laboratories and Hospitals Alike
Hurley points out that the January 2018 edition of TJC’s “Comprehensive Accreditation Manuals” already includes the updated standard and that participating ambulatory care, critical access hospitals, and hospitals were updated regarding the changes. The 2018 print editions will also include this change.
She also points out that exclusion from the standard’s requirements does not prevent hospitals from still requiring credentialing or privileging for their internal compliance processes or regulations. Quicho also emphasizes the importance of continuing to meet all CLIA requirements surrounding competencies, training, and personnel qualifications.
The TJC update should result in less action required by both clinical laboratories and hospitals alike—a welcome change for a market in a state of near-constant flux due to healthcare reform and increased regulation. The reasoning behind the decision also highlights current trends amongst pathology groups and clinical laboratories concerning scaling through consolidation and outsourcing among hospitals, ambulatory care organizations, and critical care providers.
—Jon Stone
Related Information:
Now in Effect: Change to Requirements for Credentialing, Privileging of Independent Pathologists
Credentialing and Privileging of Independent Pathologists
The Joint Commission No Longer Requires Credentialing and Privileging of Independent Pathologists—Four Things to Know