Sep 24, 2018 | Compliance, Legal, and Malpractice, Instruments & Equipment, Laboratory Instruments & Laboratory Equipment, Laboratory Management and Operations, Laboratory News, Laboratory Operations, Laboratory Pathology, Laboratory Testing, Management & Operations, News From Dark Daily
It’s the next wave in the long-running trend of hospital laboratory consolidation, as the need to trim costs and support thriving medical laboratory outreach programs continues
There’s an important new development in the hospital/health system sector of the clinical laboratory industry that continues the longstanding trend of consolidating multi-site lab operations. It is to rationalize and standardize medical laboratory operations across all lab sites within the health system. Effectively, this standardization trend represents the next cycle of clinical laboratory consolidation.
One recent example of this trend can be found at Atrium Health, the hospital health network based in Charlotte, N.C. (formerly known as Carolinas HealthCare System until earlier this year). Becker’s Hospital Review states that Atrium Health is the “seventh largest nonprofit system in the country based on number of acute-care hospitals (35).”
Creating Standardized Medical Laboratory Testing Services at Multiple Sites
Over the past four years, the clinical laboratory team at Atrium Health has worked to design, build, and operate a new, state-of-the-art core laboratory. At the same time, there were sequential projects to integrate the lab testing services and operations of nine other medical lab sites within the health system to better align the test menu, lab instruments, and workflow at these sites with the activities of the core laboratory.
According to Modena Henderson, MHA, the Vice President of Laboratory Services at Atrium Health, in an interview with Dark Daily, there were multiple primary goals in this project to rationalize and standardize lab testing at all the participating lab sites. They include:
- Standardizing lab test methodologies, reference ranges, and test menu;
- Standardizing analyzers and test platforms across all labs;
- Using Lean, Six Sigma, and other process improvement methods to streamline workflow and reduce test turnaround time;
- Improve productivity of lab staff;
- Increase quality while reducing or eliminating unproductive activities;
- Using real-time analytics middleware to keep lab management informed on a daily basis, and,
- Collaborating with emergency departments, wards, and outreach physicians to deliver more value with clinical lab testing services.
Using the ‘Three Ps of Project Management’ Approach in Health System Labs
The centerpiece of this program of lab rationalization and consolidation was the design and build-out for a new core clinical laboratory facility. Henderson said her team followed the principals of the “Three Ps of Project Management”—People, Process, Performance—to model the new lab facility, then guide how it was constructed and brought into daily clinical service.
“The Atrium Health laboratory regionalization project is an example of the next step that many innovative hospital laboratories are taking,” stated Robert L. Michel, Editor-in-Chief of The Dark Report. “Every lab has the same double challenge. First is financial. Hospital lab budgets are shrinking as growth in inpatient admissions slows. Outreach revenues are declining as Medicare and private payers slash lab test prices.
“Second, labs must come up with the capital needed to acquire and deploy the expensive and sophisticated new genetic and molecular tests that physicians and patients want,” he continued. “Hospital and health network labs must offer these new tests to keep their parent organizations at the cutting edge of clinical care.
Clinical Labs See Value in Standardizing Test Methodologies, Menus
“Thus, it is logical for the clinical labs of health networks to begin the process of rationalizing and standardizing their test menus, methodologies, and analyzers at every site within the system that performs medical lab testing,” emphasized Michel. “This is a development that we have watched gather momentum.”

Keynote Speaker Robert L. Michel, Editor-in-Chief of The Dark Report and Dark Daily will discuss how clinical laboratories of hospitals and health networks are rationalizing and standardizing their medical laboratory testing services to achieve the goals of managing lab costs, boosting quality, and increasing lab outreach revenue. The 12th annual Lab Quality Confab takes place on Oct. 9-10, 2018, at the Hyatt Regency Atlanta. (Photo copyright: The Dark Report.)
Michel offered two examples of sizable programs to rationalize and standardize clinical lab tests and services across a large health system. One is in Michigan, at Ascension Health. The other is in the Canadian Province of Québec. Both are large and ambitious undertakings, both in the number of lab sites involved and the large geography served by these clinical laboratories.
Consolidation Project in Québec involves 123 Clinical Lab Facilities
Québec’s provincial health system wants to consolidate 123 clinical laboratories in the province into 11 groups (clusters) of labs. Each lab group, or cluster, will have a core lab and rapid response labs. Test menus and methodologies will be standardized throughout the province. In an interview with The Dark Report, Ralph Dadoun, PhD, Project Director for Optilab Québec, plans to accomplish the consolidation without adding costs.
In Michigan, Ascension’s clinical lab leadership is working to integrate and standardize the labs that are operated by seven system organizations. This includes 14 hospitals and 18 existing laboratories located throughout the entire State of Michigan. In an interview with The Dark Report, Carlton Burgess, MSM, Vice President of Laboratory Services at Ascension Health’s St. John Providence Clinical Pathology Laboratory in Grosse Pointe Woods, Mich., stated that the goal is to have all the labs in the state work together in a seamless, integrated fashion.
Regional Lab Integration at North Carolina’s Biggest Health System
“To achieve this, the labs will be linked in four regions—a process we describe as regional integration,” explained Burgess. “Each region has a core lab and rapid response labs and each region will be responsible for building lab volume through increased outreach testing. In addition to changing how labs serve each region, our statewide standardization project has three objectives:
- “Repatriate existing send-out lab testing back into Michigan;
- “Establish standard test menus for each facility; and,
- “Renew each lab’s focus on growing lab outreach business.
“Every lab administrator and pathologist working in hospital and health network laboratories should be tracking this new trend of regionalization and standardization of hospital labs,” observed Michel. “That’s because labs already moving down this path are setting new standards for the entire clinical laboratory industry. This goes beyond cost and productivity, because these labs are putting the systems in place that will allow them to deliver more value to physicians and thus be paid more for that value by private health insurers.”
Innovative Lab Leaders to Speak at Lab Quality Confab in Atlanta
Lab leaders from Ascension Health will be keynote speakers at the upcoming 12th Annual Lab Quality Confab that takes place on October 9-10, 2018, at the Hyatt Hotel in Atlanta. They will also conduct multiple learning sessions to share their successes and lessons learned in building a new core laboratory and using that as a foundation to rationalize and standardize test methods, reference ranges, menus, lab automation, and analyzers at every clinical lab facility in the Ascension Health system. Sessions by Ascension Health lab leaders include:
- Leveraging Lean to become a Best-in-Class Lab Performer: How We Built and Automated a New Core Lab while Integrating Lab Operations and Helping Staff Embrace a New Culture; Modena Henderson, Vice President, Laboratory Services, and, Steven Harris, Assistant Vice President, Atrium Health.
- Achieving Standardized, High-Performance Lab Testing Services at Multiple Hospitals Using Lean Methods and Effective Engagement with Lab Staff and Nurses; Gary Catarella, MBA, MT(ASCP), Assistant Vice President, Hospital Operations, Atrium Health.
- Lessons We’ve Learned in Our Step-by-Step Journey to Transform Lab Operations and Integrate Testing across All Sites: Engaging Staff, Sustaining Change, Working with Vendors and Consultants—Interactive Roundtable Discussion; Modena Henderson, Vice President, Laboratory Services; and, Steven Harris, Assistant Vice President, Atrium Health.
Using Lean, Six, Sigma, ISO 15189 in Clinical Laboratory Operations
Lab Quality Confab this year features 60 speakers and 40 presentations from lab administrators, pathologists, and other lab managers on their successes and innovations using Lean, Six Sigma, ISO 15189, and other process management methods. You can view the full agenda here (or copy and paste this URL into your web browser: https://www.labqualityconfab.com/agenda).
This year’s Lab Quality Confab is on track to be the largest in its 12-year history. Limited spaces are still available. To ensure your place, register today at: https://www.labqualityconfab.com/register (or copy and paste this URL into your web browser: https://www.labqualityconfab.com/register).
Also, you can bring your lab team and make this Lab Quality Confab a group learning opportunity. When you bring four or more from your organization, each can register for $695 for this two-day learning event. One benefit you’ll gain from bringing your team is that it will give them the knowledge, the tools, and the confidence to help your lab reduce costs without compromising quality, while supporting sustained revenue growth from your hospital lab’s successful outreach program.
—Michael McBride
Related Information:
Full Agenda and Other Details for 12th Annual Lab Quality Confab
To Register for 12th Annual Lab Quality Confab
10 Things to Know about Atrium Health, Formerly Carolinas HealthCare System
Québec’s Laboratory Consolidation Plan Aims to Save $13.5 Million: Optilab Québec to move 123 labs into 11 lab groups
Michigan’s Ascension to Standardize Labs Throughout the State: Goals Are Common Test Methods, Menus, Practices
Sep 19, 2018 | Laboratory Management and Operations, Laboratory News, Laboratory Operations, Laboratory Pathology, Laboratory Testing, Management & Operations
As inpatient care declines, outpatient care expands, signaling a shift from where physician orders for medical laboratory tests originate
It’s a well-established fact that the year-over-year increase in the volume of outpatient procedures is consistently greater than 8%, while the annual growth in inpatient admissions is at or below 3%. Clinical laboratory managers and anatomic pathologists are aware of these facts.
MEDACorp, a strategic knowledge resource and subsidiary of Leerink Partners, a Boston-based investment bank that focuses on the healthcare industry, conducted a quarterly survey of hospital administrators from 47 hospitals in June of this year. The purpose was to evaluate healthcare utilization trends for different types of medical facilities.
According to the survey, the “ utilization trends for both [quarter-over-quarter] and [year-over-year] are decelerating across all four sites of service.” However, hospital administrators report the use of inpatient and other hospital services did not fare as well.
“The results are also modestly positive for facilities, with the slowing 0.7% increase in inpatient procedures (IP) utilization still higher than consensus of ~flat (sic) for the coverage group. Significant mix shift continues as IP mix is down and the outpatient procedure (OP) mix is up across all service lines, supporting our recent analyses of an accelerated push to ambulatory sites of service,” the survey noted.
The survey revealed:
- Inpatient services increased by just 0.7% during the second quarter of 2018, down from 1% growth during the second quarter of 2017;
- Ambulatory surgery center utilization grew by just 1.4% during the second quarter of 2018, down from 2.2% for the same quarter in 2017; and,
- Emergency department utilization increased by 0.9% in the second quarter of 2018.

“It was even weaker than many of us expected,” Ana Gupte, PhD, Managing Director, Healthcare Services at Leerink, told Modern Healthcare. “It’s pretty clear there’s no volume rebound.” (Photo copyright: Leerink.)
Inpatient Top Surgeries Predicted to Keep Moving to Outpatient Settings
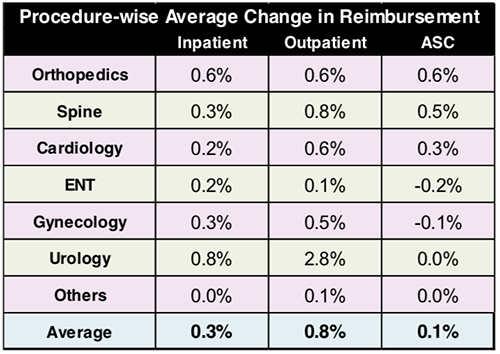
The Leerink survey found that orthopedic and cardiac procedures are leading the trend of shifting clinical procedures from inpatient to outpatient care. For example, heart surgeries were performed in outpatient settings 9% of the time over the past year and are expected to increase to 12% during the next year. Inpatient heart surgeries are expected to decrease 1% over the next year, moving from 82% to 81% of surgeries performed.
Inpatient hip procedures also are projected to drop from 77% to 75% over the course of the next year, while outpatient hip procedures are expected to increase from 17% to 19%. The survey respondents also expect other surgeries including urological, gynecological, spine and knee procedures to move to outpatient settings over the next year.
Forty-five percent of the respondents in the survey named baby boomers aging into Medicare as the most important driver of hospital utilization. Fifteen percent attributed the trend to the effects of the Affordable Care Act (ACA), and 13% cited the improving US economy as driving the use of outpatient medical facilities.
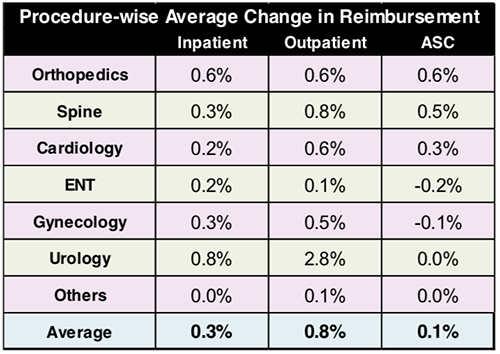
The graphic above, taken from the Leerink MEDACorp survey, illustrates a shift in healthcare procedures from inpatient to outpatient settings. Along with the surgical relocations are changes in reimbursements as well, which directly impacts clinical laboratories revenue streams and billing procedures. (Image copyright: Leerink.)
The survey respondents were from different regions and disparate population areas:
- 49% of the surveyed facilities were located in metropolitan areas;
- 40% were in suburban areas; and,
- 11% were in rural areas.
In addition:
- 32% were in the South;
- 26% were in the Northeast;
- 21% were in the Midwest; and,
- 21% were in the West.
Most of the facilities used in the survey were community hospitals, which accounted for 62% of the environments. Thirty-two percent of the facilities were academic medical centers, while the remaining 6% were other types of facilities.
The majority of the respondents for the survey were C-suite executives. In hospital settings that would include the Chief Executive Officer (CEO), Chief Financial Officer (CFO), Chief Operating Officer (COO), and other Chief titles, and, of course, hospital administrators.
Clearly, this type of downward trend could negatively impact clinical laboratories, pathology groups, and other service lines in hospital networks. Fewer patients equal less revenue for hospitals, which could eventually lead to budget cuts. A responsible medical laboratory manager will be prepared for these possibilities.
—JP Schlingman
Related Information:
Hospital Execs Say Inpatient Volume Growth Isn’t Rebounding
Hospital Utilization Slows as Healthcare Moves to Cheaper Care Settings
2Q18 Hospital Util. Survey: Utilization Decelerating, Shift To OP/ ASC Continues
ASCs Beat Inpatient Setting for Quarter, Year-over-year Utilization Increases—6 Study Insights
10 Key Trends for ASCs and Outpatient Surgery in the Next 10 Years
Sep 17, 2018 | Compliance, Legal, and Malpractice, Laboratory Management and Operations, Laboratory News, Laboratory Operations, Laboratory Pathology, Managed Care Contracts & Payer Reimbursement, Management & Operations
Ongoing federal regulatory push for EHR interoperability requires medical laboratories and anatomic pathology groups to have strategies for ensuring seamless interfaces with providers and hospitals
What difference does a name make? Clinical laboratories and anatomic pathology groups soon may know the answer to that question following the renaming of the Centers for Medicare and Medicaid Services (CMS) “Meaningful Use” program to “Promoting Interoperability” (PI).
CMS first announced the rebranding in April as part of a proposed rule aimed at transforming the Meaningful Use aspect of the federal Health Information Technology for Economic and Clinical Health (HITECH) Act. HITECH has been Medicare’s roadmap to electronic health record (EHR) implementation and interoperability since it was enacted in 2009.
The final rule arrived on August 2, 2018, and it may impact how clinical laboratories interface with provider and hospital EHRs.
Removing Obstacles to Quality Patient Care
In the news release outlining the updates to Medicare payment policies and rates under the Inpatient Prospective Payment System and the Long-Term Care Hospital Prospective Payment System, CMS states the “overhaul” of the meaningful use program will:
- Make the program more flexible and less burdensome;
- Emphasize measures that require the exchange of health information between providers and patients; and,
- Incentivize providers to make it easier for patients to obtain their medical records electronically.

“We’re excited to make these changes to ensure care will focus on the patient, not on needless paperwork,” CMS Administrator Seema Verma stated in the news release. “We’ve listened to patients and their doctors who urged us to remove the obstacles getting in the way of quality care and positive health outcomes. Today’s final rule reflects public feedback on CMS proposals issued in April and the agency’s patient-driven priorities of improving the quality and safety of care, advancing health information exchange and usability, and removing outdated or redundant regulation on healthcare providers to make way for innovation and greater value.” (Photo copyright: Centers for Medicare and Medicaid Services.)
According to a CMS fact sheet, key provisions of the overhaul include:
- The rule finalized an EHR reporting period to a minimum of any continuous 90-day period in each of calendar years 2019 and 2020 for new and returning participants attesting to CMS or their State Medicaid agency;
- For the Medicare Promoting Interoperability Program, the rule finalized a new performance-based scoring methodology consisting of a smaller set of objectives that CMS states will provide a more flexible, less-burdensome structure, allowing eligible hospitals and critical access hospitals (CAHs) to place their focus back on patients;
- CMS finalized two new e-Prescribing measures related to e-prescribing of opioids (Schedule II controlled substances); and,
- Beginning with an EHR reporting period in CY 2019, all eligible hospitals and CAHs under the Medicare and Medicaid PI programs will be required to use the 2015 Edition of Certified EHR Technology;
- CMS finalized changes to measures, including removing certain measures CMS believes do not emphasize interoperability and the electronic exchange of health information.
According to CMS, about 3,300 acute care hospitals and 420 long-term care hospitals will be subject to the final rule, which takes effect October 1. Obviously, medical laboratories servicing these healthcare organizations will be similarly affected.
Rebranding More than a Name Change
Healthcare Informatics analyzed the 2,593-page final rule explaining that the “core emphasis” of the meaningful use overhaul is “on advancing health data exchange among providers.”
The initial proposal in April, according to Healthcare Informatics, invited stakeholder feedback through a request for information on the possibility of revising CMS’ “Conditions of Participation” for hospitals by requiring providers to electronically transfer medically necessary information following a patient discharge or transfer. The final rule, however, did not include that change.
Instead, the CMS Fact Sheet on the rule states the April request for information was “to obtain feedback on positive solutions to better achieve interoperability, or the sharing of healthcare data between providers, which will inform next steps in advancing this critical initiative.”
Rebranding meaningful use is CMS’s first step in implementing core pieces of the Administration’s MyHealthEData Initiative to strengthen interoperability. In remarks during the ONC Interoperability Forum in Washington, DC, CMS Administrator Seema Verma described the rebranding decision as “much more than a name change” and signaled future CMS actions.
“It is a change in direction for the programs—from programs that support the adoption of health IT, to programs that promote interoperability and patient access to data,” she explained. “To avoid payment reductions and gain incentives, doctors and hospitals will have to give patients electronic access to their health records. We are also considering whether CMS should require—as a condition of participation in the Medicare program—that providers share data with patients in a universal electronic format and hope to share more information on that soon.”
The recent changes follow passage of the Bipartisan Budget Act of 2018, which included a provision relaxing meaningful-use requirements. Though the legislation affects only hospitals and outpatient Medicaid providers, Robert Tennant, Director of Health Information Technology Policy for the Medical Group Management Association (MGMA), declared the revision a “huge win” for providers.
“I don’t think the government recognized how difficult it would be to move from stage 1 to stage 2 to stage 3 [meaningful use] requirements and the significant costs involved,” Tennant stated told Modern Healthcare. “We hope that it signals an interest in Congress in having the administration and HHS (Federal Health and Human Services) not make these quality reporting programs so onerous that it results in large swaths of providers not being successful.”
Clinical laboratories and anatomic pathology groups should be aware that interoperability between their laboratory information systems and the EHRs of providers and hospitals continues to be important. Although the term “Meaningful Use” is to be supplanted by “Promoting Interoperability,” the ability to move patient health information seamlessly among providers continues to be a major goal of this country’s healthcare system.
—Andrea Downing Peck
Related Information:
CMS Finalizes Changes to Empower Patients and Reduce Administrative Burden
In Proposed MU Rebranding Rule, CMS Raises the Interoperability Stakes
Fact Sheet: Fiscal Year (FY) 2019 Medicare Hospital Inpatient Prospective Payment System (IPPS) and Long-Term Acute Care Hospital (LTCH) Prospective Payment System Final Rule (CMS-1694-F)
H.R. 1892: Bipartisan Budget Act of 2018
Printable PDF: Final Rule (CMS-1694-F)
Speech: Remarks by Administrator Seema Verma at the ONC Interoperability Forum in Washington, DC
Congress Budget Deal Relaxes Meaningful-Use Requirements
CMS Proposes Changes to Empower Patients and Reduce Administrative Burden
CMS Proposes Meaningful Use Changes to Promote Interoperability
Sep 14, 2018 | Compliance, Legal, and Malpractice, Laboratory Management and Operations, Laboratory News, Laboratory Operations, Laboratory Pathology, Management & Operations
Defamation, libel, harassment, and causing emotional distress are some of the charges patients who launched online negative review campaigns are defending themselves against in court
Healthcare systems, surgeons, family practitioners, clinical laboratories, anatomic pathologists—none are immune to receiving negative online reviews from patients who believe they’ve been damaged by their caregivers. And these reviews can have such an impact on practice revenues, doctors and hospitals have begun suing patients for damages caused by harmful online reviews. And they are winning.
Several notable cases involve high-profile healthcare systems. One such lawsuit involved the Cleveland Clinic. A patient who claimed a 2008 prostate surgery left him impotent and incontinent due to negligence on the part of the surgeon launched a negative campaign that spanned a decade, USA Today reported.
David Antoon, a retired Air Force Colonel, filed a malpractice lawsuit against urologist, Jihad Kaouk, MD, and the Cleveland Clinic. Antoon alleged Kaouk was not present in the operating room during his surgery, even though he insisted that only Kaouk perform the procedure. Antoon also claimed the Cleveland Clinic’s urology department did not have the proper credentials to operate the robotic device used during his surgery.
In addition to filing the lawsuit, Antoon complained to the federal Centers for Medicare and Medicaid Services (CMS) and the State Medical Board of Ohio.
However, Antoon also vented his frustrations on social media, as well as sending e-mails to Kaouk, which the doctor felt were threatening and made him concerned about the situation escalating. “What would be next—showing up at my door?” Kaouk asked during the criminal trial against Antoon. “That’s what we feared.”

Jihad Kaouk, MD (above), a urologist with the Cleveland Clinic, giving testimony at Cuyahoga County Common Pleas Court during a lawsuit involving patient David Antoon, a retired Air Force Colonel. Kaouk and the Cleveland Clinic prevailed in that lawsuit and the State Medical Board of Ohio closed a five-year investigation into Kaouk without reprimanding him. (Photo copyright: USA Today.)
Antoon posted unfavorable online comments about Kaouk for a decade. The urologist eventually petitioned the court, which granted him a civil stalking protective order against Antoon. It banned Antoon from contacting the doctor. Nevertheless, the day after that order was granted, Antoon posted another bad review about Kaouk on Yelp and urged people to avoid Kaouk when seeking medical care.
Antoon was later arrested on felony charges of menacing by stalking, telecommunications harassment, and violating a protection order. He faced up to one year in prison if indicted. In addition to spending two days in jail, he paid $40,000 for a defense attorney and a $50,000 bond after being arrested. He also agreed to pay $100 as part of a plea deal.

Above is David Antoon (left), Col USAF Ret, and Don Malarcik (right), an attorney with Malarcik, Pierce, Munyer, and Will in Akron, Ohio. Malarcik argued that “the Yelp review doesn’t violate the protection order because Antoon did not make direct contact with Kaouk,” Cleveland.com reported. (Photo copyright: USA Today.)
Other Lawsuits Against Patients Involving Social Media
Joon Song, MD, PhD, a New York City area gynecologist sued patient Michelle Levine over critical reviews she left about his practice on several online sites. Though Levine removed her posts from the sites after being sued, Song wants her to pay $1 million in legal fees and damages. The doctor accused Levine of defamation, libel, and causing emotional distress. Sound familiar?
Two Scottsdale, Ariz., doctors—Albert Carlotti, MD, and Michelle Cabret-Carlotti, MD, DDS,—successfully sued patient Sherry Petta for defamation after she posted negative statements about the doctors online. After filing a complaint with the Arizona Medical Board and clashing with Carlotti over access to her medical records, Petta posted unfavorable reviews about the practice on several online sites and created a website to warn others about Carlotti. The doctors claimed the statements Petta made were untrue and portrayed them in a false light. A jury agreed and awarded the doctors $12 million, which was later vacated on appeal.
Cleveland cosmetic surgeon Bahman Guyuron, MD, sued a former patient after she posted adversarial reviews on several online review sites about her dissatisfaction with a nose job. The patient, who remains unidentified, alleges that Guyuron acted in an untrustworthy and unprofessional manner, that she received no follow-up care, and that Guyuron urges people to post erroneous positive reviews online. She also claims that there was no informed consent to the procedure and that her nose is now twice as large as before.
Guyuron is seeking monetary damages, an injunction against the patient to prevent her from posting negative reviews about him online, and an order to remove all existing statements about him from the Internet.
Clinical Laboratories Vulnerable to Negative Reviews
Healthcare is complicated and positive outcomes can never be guaranteed. When patients do not get satisfaction by complaining to the doctors and facilities, they may seek other ways to be heard. And negative comments made on social media and online review websites can harm the reputations and businesses of physicians and medical facilities.
“It would be great if the regulators of hospitals and doctors were more diligent about responding to harm to patients, but they’re not, so people have turned to other people,” Lisa McGiffert, former head of the Consumer Reports Safe Patient Project, told USA Today. “This is what happens when your system of oversight is failing patients.”
However, Ryan Lorenz, Petta’s attorney warns consumers to be aware of the consequences of posting critical online reviews, especially if they post factually inaccurate information. “Make sure what you are saying is true—it has to be truthful,” he told USA Today.
Similar situations can arise in the clinical laboratory industry as well. There were multiple postings on Yelp in 2014 and 2015 by patients criticizing blood-testing company Theranos regarding discordant test results they’d received from Theranos’ lab, which Dark Daily covered in multiple e-briefings.
Trust is the hardest thing to earn, the easiest thing to lose, and once gone, can be impossible to get back. Clinical laboratories are just as susceptible to negative reviews as hospitals and doctors.
Worse yet, labs can be drawn into lawsuits simply because they service the hospital systems and caregivers involved. Preparing in advance for this possibility should be on every clinical laboratory manager’s do list.
—JP Schlingman
Related Information:
Doctors, Hospitals Sue Patients Who Post Negative Comments, Reviews on Social Media
Doctor Sues Patient for $1 Million for Posting Negative Reviews Online
I Wrote a Negative Yelp Review—and it Made My Life a Nightmare
Hospital Sues Over Facebook Post and Picketing
Previously High-Flying Theranos Provides Clinical Laboratories and Pathology Groups with Valuable Lesson on How Quickly Consumer Trust Can Be Lost
Federal Appeals Court Rules Yelp Not Responsible for Bad Reviews; Labs Advised to Examine Their Online Presence
Online Negative Reviews Can Threaten Clinical Laboratories Not Prepared to Address Feedback or Manage Their Internet Presence
Sep 12, 2018 | Laboratory Management and Operations, Laboratory News, Laboratory Operations, Laboratory Pathology, Management & Operations
Contrary to CMS and Joint Commission programs implemented in 2017 to reduce them, incidents of hospital-acquired infections have risen for the past few years
Clinical laboratories and anatomic pathologists know that hospital-acquired infections (HAIs) can be deadly, not just for patients, but for their caregivers and families as well. Even one HAI is too many. Thus, the federal Centers for Medicare and Medicaid Services (CMS) required healthcare organizations to upgrade their antimicrobial stewardship (AMS) programs to meet CMS requirements and Joint Commission accreditation starting in 2017.
Nevertheless, a recent Leapfrog Group report indicates hospitals are finding it increasingly difficult to remove infections all together. This has many healthcare leaders concerned.
The report, which was analyzed by Castlight Health, states that the number of hospitals reporting zero infections has declined significantly since 2015, according to a news release. According to the Leapfrog Group’s report:
- Two million people acquire HAIs every year;
- 90,000 people die annually from HAIs;
- HAI costs range from $1,000 to $50,000 depending on the infection.
Hospitals spend $28 to $45 billion annually on HAI costs, Healthcare Finance reported.

“I think it’s far too easy to let something slip, so it’s clear that there really needs to be a renewed focus on getting back to zero. We do still see some hospitals that are getting to zero, so it’s clearly possible,” Erica Mobley (above), Leapfrog Group’s Director of Operations, told Fierce Healthcare. (Photo copyright: LinkedIn.)
Regressing Instead of Progressing Toward Total HAI Elimination
Leapfrog Group’s report is based on 2017 hospital survey data submitted by 2,000 providers. The data indicates that in just two years the number of hospitals reporting zero HAIs dropped by up to 50%. The reported HAIs include:
The remaining infection measures studied by Leapfrog Group had less dramatic decreases over the same time period, according to Fierce Healthcare. Nevertheless, they are significant. They include:
- Surgical site infections (SSI) following colon surgery: 19% zero infections compared to 23% previously;
- Clostridium difficile (C. difficile) inpatient infections: 3% zero inpatient infections in 2017, compared to 5% in 2015.
Joint Commission Studies Antimicrobial Program Progress
Meanwhile, the Joint Commission acknowledged that implementation of antimicrobial stewardship programs by providers can be difficult. In “The Expanding Role of Antimicrobial Stewardship Programs in Hospitals in the United States: Lessons Learned from a Multisite Qualitative Study,” the accrediting organization released insights from interviews with 12 antimicrobial stewardship program leaders nationwide.
They published their study in “The Joint Commission Journal on Quality and Patient Safety.” Three themes emerged from the interviews:
- Hospitals have revised their antimicrobial programs, which originally operated on a “top-down” structure, to programs that include clinicians from throughout entire provider organizations;
- Health information technology (HIT) can enable real-time opportunities to launch antimicrobial therapy and treat patients; and,
- Some barriers exist in getting resources to integrate technology and analyze data.
“These programs used expansion of personnel to amplify the antimicrobial stewardship programs’ impact and integrated IT resources into daily workflow to improve efficiency,” the researchers wrote. “Hospital antimicrobial stewardship programs can reduce inappropriate antimicrobial use, length of stay, C. difficile infection, rates of resistant infections, and cost.”
What Do CMS and Joint Commission Expect?
According to Contagion, while the Joint Commission program is part of medication management, CMS places its requirements for the antimicrobial stewardship program under “infection prevention.”
CMS requirements for an antimicrobial stewardship program include:
- Developing antimicrobial stewardship program policies and procedures;
- Implementing hospital-wide efforts;
- Involving antimicrobial stakeholders for focus on antimicrobial use and bacterial resistance;
- Setting evidence-based antimicrobial use goals; and,
- Reducing effects of antimicrobial use in areas of C. difficile infections and antibiotic resistance.
Leapfrog Group’s data about fewer hospitals reporting zero infections offers opportunities for hospital laboratory microbiology professionals to get involved with hospital-wide antimicrobial program teams and processes and help their hospitals progress back to zero HAIs. Clinical laboratories, both hospital-based and independent, also have opportunities to contribute to improving the antimicrobial stewardship efforts of the physicians who refer them specimens.
—Donna Marie Pocius
Related Information:
Troubling New Report on Hospital Infections Comes While Centers Medicare and Medicaid Services Considers Discontinuing Publicly Reporting Rates
Leapfrog Group: Healthcare-Associated Infections
Antimicrobial Stewardship Standards: A Comparison of Centers for Medicare and Medicaid Services and Joint Commission Requirements
Joint Commission: New Antimicrobial Stewardship Standard
Core Elements of Hospital Antibiotic Stewardship Programs
Number of Hospitals Achieving Zero Infections Drops
Hospitals Losing Ground on Effectively Preventing Infections with Dramatic Drop in Those Reporting Zero Infections
The Expanding Role of Antimicrobial Stewardship Programs in Hospitals in the United States: Lessons Learned from a Multi-Site Qualitative Study
Sep 10, 2018 | Laboratory Management and Operations, Laboratory News, Laboratory Operations, Laboratory Pathology, Laboratory Testing, Management & Operations
Clinical laboratory test claims make up a substantial proportion of all claims filed each year. Thus, any effort to streamline or reform claims adjudication and administration in the US will alter how labs and pathologists conduct business
Clinical laboratory managers and anatomic pathologists know how costly and complex the US healthcare system can be. However, expenses associated with care and treatment are only part of the total picture. Resources devoted to paperwork and administrative costs apparently increase overall expenditures associated with healthcare to a much higher degree than is generally known.
That’s according to several studies The New York Times reported on in July.
US Administrative Costs Higher than All Other Nations
One study conducted by The New England Journal of Medicine (NEJM) in 2003 estimated administrative costs account for approximately 30% of all healthcare expenditures in the US. The researchers examined data from 1999 to reach those conclusions. In today’s economy, those numbers are higher. On average, $5,700 of every $19,000 that US workers and their employers pay for family coverage each year goes towards administrative costs.
A 2014 study published by Health Affairs compared administrative costs for US hospital expenditures to those of seven other countries: Canada, England, France, Germany, the Netherlands, Scotland, and Wales. This study evaluated data from 2010/2011 and found that hospital administrative costs in the US far exceed rates in other nations. According to the study, administrative costs accounted for:
- 25.3% of total hospital expenditures in the US;
- 19.8% in the Netherlands;
- 15.5% in England; and,
- 12% in Canada and Scotland.
According to the Health Affairs study, more than $150 billion could have been saved in 2011 by reducing per capita spending for administrative costs to the levels observed in Canada and Scotland.

“The extraordinary costs we see are not because of administrative slack or because healthcare leaders don’t try to economize,” Kevin Schulman, MD, Professor, Department of Medicine, Duke University, and co-author of the Health Affairs study told The New York Times. “The high administrative costs are functions of the system’s complexity.” (Photo copyright: Duke University.)
Complexity of Payer System Partly to Blame
One reason for the costliness in the US healthcare system is the myriad of payers that healthcare organizations have to grapple with to receive payment. Private health insurers and public health programs like Medicare and Medicaid, each have their own procedures, regulations, and forms that need to be submitted to receive payments. This translates to more employee time devoted to billing.
Another factor driving costs is the staff time devoted to the collection of debts. A 2017 Health Affairs study examined medical claims data from 88,000 healthcare providers contracted with Athenahealth to determine the percentage of bills paid within one year from the initial service.
The study found that 93.8% of patient bills under $35 were paid within a year. However, that percentage decreased as the patient obligation increased:
- 90.5% of patients paid bills between $35 and $75 within one year;
- 83.7% paid bills between $75 and $200 in the same time period; however,
- When bills increase to $200 or more, just 66.7% were paid within a year’s time.
Providers wrote off approximately 16% as abandoned or bad debts, with an additional 17% going to collection agencies.
Another study, published in Health Affairs in 2009, surveyed 895 physicians about the time they spent dealing with administrative tasks. On average, physicians reported spending 43 minutes per workday interacting with health plans. This number is the equivalent of three hours/week and almost three weeks/year. Those numbers have reportedly increased since then.
EHRs Do Not Reduce Administrative Costs, Contrary to Belief
Efforts have been made to reduce administrative costs in the US healthcare industry. One such measure involved increased use of certified electronic health record (EHR) systems, which the federal government spent billions of dollars promoting and incentivizing providers to adopt on the claim that EHRs would reduce healthcare costs, in part by removing most of the paperwork.
However, a 2018 study published in the Journal of the American Medical Association (JAMA) reported the adoption of EHRs did not reduce administration costs. Researchers at Duke University and Harvard Business School utilized a cutting-edge accounting method to determine the administrative costs within a large academic healthcare system that was using a certified EHR.
Their study determined the administrative costs for processing a single medical bill ranged from $20 for a doctor visit to $215 for an inpatient surgical procedure. These costs accounted for 3%-25% of total professional revenue for the provided services.
“We need to understand better how complexity is driving these enormous costs within the system, costs that do not add value to patients, employers, or providers,” noted Barak Richman, JD, PhD, Duke University School of Law and Margolis Center for Health Policy, one of the study’s authors.
Clinical Lab Test Claims a Major Portion of Administrative Costs
Nevertheless, administrative costs are a necessary part of doing business and not always as negative as perceived. An article published by Health Affairs in 1992 divided administrative costs in the healthcare industry into four categories:
- Transaction-related: claims processing, billing, admissions, and tracking employee hiring/terminations;
- Benefits Management: quality assurance, plan design, statistical and internal analyses, and management information systems;
- Selling and Marketing: strategic planning, underwriting, and advertising; and,
- Regulatory and Compliance: waste management, licensing requirements, and discharge planning.
“We hope that this work is the first step toward informing policy solutions that could reduce these non-value-added costs largely hidden within the healthcare system,” Schulman stated in a Duke University news release.
The issue of costly paperwork and administrative expenditures is significant for the clinical laboratory profession as lab test claims make up a substantial portion of all medical claims filed annually. Efforts to streamline or reform claims adjudication and administration will have an impact on the way clinical labs and anatomic pathology groups conduct business in the future.
—JP Schlingman
Related Information:
Hidden from View: The Astonishingly High Administrative Costs of U.S. Health Care
NEJM: Costs of Health Care Administration in the United States and Canada
Heath Affairs: A Comparison of Hospital Administrative Costs in Eight Nations: US Costs Exceed All Others by Far
Heath Affairs: Inside the Black Box of Administrative Costs
Heath Affairs: As Patients Take on More Costs, Will Providers Shoulder the Burden?
Heath Affairs: What Does It Cost Physician Practices to Interact with Health Insurance Plans?
Electronic Health Records Don’t Reduce Administrative Costs
Simplifying Administration of Health Insurance