Gates Foundation, Chan Zuckerberg Initiative Fund Open-Source Global Disease Tracker; May Be Useful Resource for Microbiology Laboratories
Cloud-based platform—IDseq—shows potential to track the causes and spread of infectious diseases worldwide using metagenomic data Here’s the latest example of how big data and related technologies can give physicians—as well as microbiologists and clinical pathologists—a new tool for understanding infectious disease and tracking outbreaks anywhere in the world. This project is being funded and organized by well-known Silicon Valley entrepreneurs. The project is known as IDseq. It was announced...The Problems with Ancestry DNA Analyses
Diagnostic medical laboratories may sequence DNA genetic tests correctly, but there are issues with how companies analyze the information
In 2017, some 12 million people paid to spit in a tube and have their genetic data analyzed, according to Technology Review. Many companies offer this type of DNA testing, and each of them works with one or more clinical laboratories to get the actual sequencing performed. For example, Ancestry.com, one of the largest direct-to-consumer genetic data testing companies, works with both Quest Diagnostics and Illumina.
In the case of Quest Diagnostics, the clinical laboratory company does the actual sequencing for Ancestry. But the analysis of the genetic data for an individual and its interpretation is performed by Ancestry’s team.
There are critics of the booming direct-to-consumer genetic testing business, but it’s not due to the quality of the sequencing. Rather, critics cite other issues, such as:
- Privacy concerns;
- How the physical samples are stored and used;
- Who owns the data; and,
- That this branch of genetics is an area of emerging study and not clearly understood.
What Does All That Genetic Data Mean?
The consumer DNA testing market was worth $359 million dollars in 2017 and is projected to grow to $928 million by 2023, according to a report from Research and Markets. Those numbers represent a lot of spit, and an enormous amount of personal health information. As of now, some one in every 25 adults in the US has access to their genetic data. But, what does all that data mean?
The answer depends, in large part, on who you ask. Many reporters, scientists, and others have taken multiple DNA tests from different companies and received entirely different results. In some cases, the sequencing from one sample submitted to different companies for analysis have rendered dramatically different results.

“There is a wild-west aspect to all of this,” Erin Murphy, a New York University law professor and genetics specialist who focuses on privacy implications, told McClatchy. “It just takes one person in a family to reveal the genetic information of everyone in the family,” she notes. (Photo copyright: New York University.)
It’s All About the Database
Although some people purchase kits from multiple companies, the majority of people take just one test. Each person who buys genetic analysis from Ancestry, for example, consents to having his/her data become part of Ancestry’s enormous database, which is used to perform the analyses that people pay for. There are some interesting implications to how these databases are built.
First, they are primarily made up of paying customers, which means that the vast majority of genetic datasets in Ancestry’s database come from people who have enough disposable income to purchase the kit and analysis. It may not seem like an important detail, but it shows that the comparison population is not the same as the general population.
Second, because the analyses compare the sample DNA to DNA already in the database, it matters how many people from any given area have taken the test and are in the database. An article in Gizmodo describes one family’s experience with DNA testing and some of the pitfalls. The author quotes a representative from the company 23andMe as saying, “Different companies have different reference data sets and different algorithms, hence the variance in results. Middle Eastern reference populations [for example] are not as well represented as European, an industry-wide challenge.”
The same is true for any population where not many members have taken the test for a particular company. In an interview with NPR about trying to find information about her ancestry, journalist Alex Wagner described a similar problem, saying, “There are not a lot of Burmese people taking DNA tests … and so, the results that were returned were kind of nebulous.”
Wagner’s mother and grandmother both immigrated to the US from Burma in 1965, and when Wagner began investigating her ancestry, she, both of her parents, and her grandmother, all took tests from three different direct-to-consumer DNA testing companies. To Wagner’s surprise, her mother and grandmother both had results that showed they were Mongolian, but none of the results indicated Burmese heritage. In the interview she says that one of the biggest things she learned through doing all these tests was that “a lot of these DNA test companies [are] commercial enterprises. So, they basically purchase or acquire DNA samples on market-demand.”
As it turns out, there aren’t many Burmese people taking DNA tests, so there’s not much reason for the testing companies to pursue having a robust Burmese or even Southeast Asian database of DNA.
Who Owns Your Genetic Data?
As is often the case when it comes to technological advances, existing law hasn’t quite caught up with the market for ancestry DNA testing. There are some important unanswered questions, such as who owns the data that results from a DNA analysis?
An investigation conducted by the news organization McClatchy found that Ancestry does allow customers to request their DNA information be deleted from the company’s database, and that they can request their physical sample be destroyed as well. The author writes, “But it is a two-step process, and customers must read deep into the company’s privacy statement to learn how to do it. Requests for DNA data elimination can be made online, but the company asks customers to call its support center to request destruction of their biological sample.”
Another concern is hacking or theft. Ancestry and similar companies take steps to protect customers’ information, such as using barcodes rather than names and encryption when samples are sent to labs. Nevertheless, there was an incident in 2017 in which hackers infiltrated a website owned by Ancestry called RootsWeb. “The RootsWeb situation was certainly unfortunate,” Eric Heath, Ancestry’s Chief Privacy Officer, told McClatchy. He added that RootsWeb was a “completely separate system” from the Ancestry database that includes DNA information.
What We Don’t Know
The biggest pitfall for consumers may be that geneticists don’t know very much about DNA analysis. Adam Rutherford, PhD, is a British geneticist who interviewed for the Gizmodo story. He said that the real problem with companies like Ancestry is that people have a basic, fundamental misunderstanding of what can be learned from a DNA test.
“They’re not telling you where your DNA comes from in the past. They’re telling you where on Earth your DNA is from today,” Rutherford told Gizmodo.
Science evolves, of course, and genetic testing has much evolving to do. The author of the Gizmodo piece writes, “It’s not that the science is bad. It’s that it’s inherently imperfect.” There aren’t any best-practices for analyzing DNA data yet, and companies like Ancestry aren’t doing much to make sure their customers understand that fact.
Nevertheless, issues surrounding genetic testing, the resulting data, and its storage, interpretation, and protection, continue to impact clinical laboratories and anatomic pathology groups.
—Dava Stewart
Related Information:
2017 Was the Year Consumer DNA Testing Blew Up
Quest Diagnostics and Ancestry DNA Collaborate to Expand Consumer DNA Testing
Illumina, Secret Giant of DNA Sequencing, Is Bringing Its Tech to the Masses
How DNA Testing Botched My Family’s Heritage, and Probably Yours, Too
A Journalist Seeks Out Her Roots but Finds Few Answers in the Soil
Ancestry Wants Your Spit, Your DNA and Your Trust. Should You Give Them All Three?
Genetic Testing as Part of Primary Care and Precision Medicine is Underway at NorthShore University HealthSystem and Geisinger Health
Both health systems will use their EHRs to track genetic testing data and plan to bring genetic data to primary care physicians
Clinical laboratories and pathology groups face a big challenge in how to get appropriate genetic and molecular data into electronic health record (EHR) systems in ways that are helpful for physicians. Precision medicine faces many barriers and this is one of the biggest. Aside from the sheer enormity of the data, there’s the question of making it useful and accessible for patient care. Thus, when two major healthcare systems resolve to accomplish this with their EHRs, laboratory managers and pathologists should take notice.
NorthShore University HealthSystem in Illinois and Geisinger Health System in Pennsylvania and New Jersey are working to make genetic testing part of primary care. And both reached similar conclusions regarding the best way for primary care physicians to make use of the information.
One area of common interest is pharmacogenomics.
At NorthShore, two genetic testing programs—MedClueRx and the Genetic and Wellness Assessment—provide doctors with more information about how their patients metabolize certain drugs and whether or not their medical and family histories suggest they need further, more specific genetic testing.
“We’re not trying to make all of our primary care physicians into genomic experts. That is a difficult strategy that really isn’t scalable. But we’re giving them enough tools to help them feel comfortable,” Peter Hulick, MD, Director of the Center for Personalized Medicine at NorthShore, told Healthcare IT News.
Conversely, Geisinger has made genomic testing an automated part of primary care. When patients visit their primary care physicians, they are asked to sign a release and undergo whole genome sequencing. An article in For the Record describes Geisinger’s program:
“The American College of Medical Genetics and Genomics classifies 59 genes as clinically actionable, with an additional 21 others recommended by Geisinger. If a pathogenic or likely pathogenic variant is found in one of those 80 genes, the patient and the primary care provider are notified.”
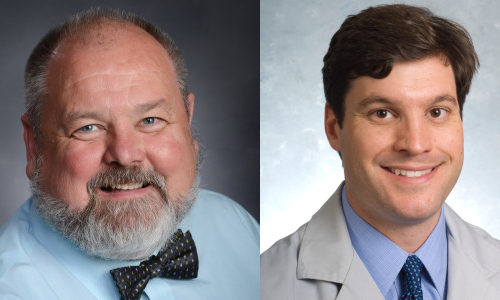
William Andrew Faucett (left) is Director of Policy and Education, Office of the Chief Scientific Officer at Geisinger Health; and Peter Hulick, MD (right), is Director of the Center for Personalized Medicine at NorthShore University HealthSystem. Both are leading programs at their respective healthcare networks to improve precision medicine and primary care by including genetic testing data and accessibility to it in their patients’ EHRs. (Photo copyrights: Geisinger/NorthShore University HealthSystem.)
The EHR as the Way to Access Genetic Test Results
Both NorthShore and Geisinger selected their EHRs for making important genetic information accessible to primary care physicians, as well as an avenue for tracking that information over time.
Hulick told Healthcare IT News that NorthShore decided to make small changes to their existing Epic EHR that would enable seemingly simple but actually complex actions to take place. For example, tracking the results of a genetic test within the EHR. According to Hulick, making the genetic test results trackable creates a “variant repository,” also known as a Clinical Data Repository.
“Once you have that, you can start to link it to other information that’s known about the patient: family history status, etc.,” he explained. “And you can start to build an infrastructure around it and use some of the tools for clinical decision support that are used in other areas: drug/drug interactions, reminders for flu vaccinations, and you can start to build on those decision support tools but apply them to genomics.”
Like NorthShore, Geisinger is also using its EHR to make genetic testing information available to primary care physician when a problem variant is identified. They use EHR products from both Epic and Cerner and are working with both companies to streamline and simplify the processes related to genetic testing. When a potentially problematic variant is found, it is listed in the EHR’s problem list, similar to other health issues.
Geisinger has developed a reporting system called GenomeCOMPASS, which notifies patients of their results and provides related information. It also enables patients to connect with a geneticist. GenomeCOMPASS has a physician-facing side where primary care doctors receive the results and have access to more information.
Andrew Faucett, Senior Investigator (Professor) and Director of Policy and Education, Office of the Chief Scientific Officer at Geisinger, compares the interpretation of genetic testing to any other kind of medical testing. “If a patient gets an MRI, the primary care physicians doesn’t interpret it—the radiologist does,” adding, “Doctors want to help patients follow the recommendations of the experts,” he told For the Record.
The Unknown Factor
Even though researchers regularly make new discoveries in genomics, physicians practicing today have had little, if any, training on how to incorporate genetics into their patients’ care. Combine that lack of knowledge and training with the current lack of EHR interoperability and the challenges in using genetic testing for precision medicine multiply to a staggering degree.
One thing that is certain: the scientific community will continue to gather knowledge that can be applied to improving the health of patients. Medical pathology laboratories will play a critical role in both testing and helping ensure results are useful and accessible, now and in the future.
—Dava Stewart
Related Information:
Introducing “Genomics and Precision Health”
How NorthShore Tweaked Its Epic EHR to Put Precision Medicine into Routine Clinical Workflows
Broad Institute/Massachusetts General Hospital Researchers Develop Multi-Gene Test That Identifies Those at High Risk for Developing Heart Disease and Four Other Potentially Deadly Conditions
Next step is to design Web portal offering low-cost ‘polygenic risk score’ to people willing to upload genetic data received from DNA testing companies such as 23andMe
Pathologists and other medical professionals have long predicted that multi-gene diagnostics tests which examine thousands of specific gene sequences might one day hold the key to assessing disease risk, diagnosing diseases, and guiding precision medicine treatment decisions. Now, a research team from the Broad Institute, Massachusetts General Hospital (MGH) and Harvard Medical School have brought that prediction closer to reality.
Their study, published last month in Nature Genetics, found that a genome analysis called polygenic risk scoring can identify individuals with a high risk of developing one of five potentially deadly diseases:
- Coronary artery disease;
- Atrial fibrillation;
- Type 2 diabetes;
- Inflammatory bowel disease; and,
- Breast cancer.
Polygenic Scoring Predicts Risk of Disease Among General Population
To date, most genetic testing has been “single gene,” focusing on rare mutations in specific genes such as those causing sickle cell disease or cystic fibrosis. This latest research indicates that polygenic predictors could be used to discover heightened risk factors in a much larger portion of the general population, enabling early interventions to prevent disease before other warning signs appear. The ultimate goal of precision medicine.
“We’ve known for long time that there are people out there at high risk for disease based just on their overall genetic variation,” senior author Sekar Kathiresan, MD, co-Director of the Medical and Population Genetics Program at the Broad Institute, and Director, Center for Genomic Medicine at Massachusetts General Hospital, said in a Broad Institute news release. “Now, we’re able to measure that risk using genomic data in a meaningful way. From a public health perspective, we need to identify these higher-risk segments of the population, so we can provide appropriate care.”

“What I foresee is in five years, each person will know this risk number—this ‘polygenic risk score’—similar to the way each person knows his or her cholesterol,” Sekar Kathiresan, MD (above), Co-Director of the Medical and Population Genetics Program at the Broad Institute, and Director, Center for Genomic Medicine at Massachusetts General Hospital, told the Associated Press (AP). He went on to say a high-risk score could lead to people taking other steps to lower their overall risk for specific diseases, while a low-risk score “doesn’t give you a free pass” since an unhealthy lifestyle can lead to disease as well. (Photo copyright: Massachusetts General Hospital.)
The researchers conducted the study using data from more than 400,000 individuals in the United Kingdom Biobank. They created a risk score for coronary artery disease by looking for 6.6 million single-letter genetic changes that are more prevalent in people who have had early heart attacks. Of the individuals in the UK Biobank dataset, 8% were more than three times as likely to develop the disease compared to everyone else, based on their genetic variation.
In absolute terms, only 0.8% of individuals with the very lowest polygenic risk scores had coronary artery disease, compared to 11% for people with the highest scores, the Broad Institute news release stated.
“The results should be eye-opening for cardiologists,” Charles C. Hong, MD, PhD, Director of Cardiovascular Research at the University of Maryland School of Medicine, told the AP. “The only disappointment is that this score applies only to those with European ancestry, so I wonder if similar scores are in the works for the large majority of the world population that is not white.”
In its news release, the Broad Institute noted the need for additional studies to “optimize the algorithms for other ethnic groups.”
The Broad Institute’s results suggest, however, that as many as 25 million people in the United States may be at more than triple the normal risk for coronary artery disease. And millions more may be at similar elevated risk for the other conditions, based on genetic variations alone.
Reanalyzing Data from DNA Testing Companies
The researchers are building a website that would enable users to receive a low-cost polygenic risk score—such as calculating inherited risk score for many common diseases—by reanalyzing data users previously receive from DNA testing companies such as 23andMe.
Kathiresan told Forbes his goal is for the 17 million people who have used genotyping services to submit their data to the web portal he is building. He told the magazine he’s hoping “people will be able to get their polygenic scores for about as much as the cost of a cholesterol test.”
Some Experts Not Impressed with Broad Institute Study
But not all experts believe the Broad Institute/MGH/Harvard Medical School study deserves so much attention. Ali Torkamani, PhD, Director of Genomics and Genome Informatics at the Scripps Research Translational Institute, offered a tepid assessment of the Nature Genetics study.
In an article in GEN that noted polygenic risk scores were receiving “the type of attention reserved for groundbreaking science,” Torkamani said the recent news is “not particularly” a big leap forward in the field of polygenic risk prediction. He described the results as “not a methodological advance or even an unexpected result,” noting his own group had generated similar data for type 2 diabetes in their analysis of the UK dataset.
Nevertheless, Kathiresan is hopeful the study will advance disease treatment and prevention. “Ultimately, this is a new type of genetic risk factor,” he said in the news release. “We envision polygenic risk scores as a way to identify people at high or low risk for a disease, perhaps as early as birth, and then use that information to target interventions—either lifestyle modifications or treatments—to prevent disease.”
This latest research indicates healthcare providers could soon be incorporating polygenic risking scoring into routine clinical care. Not only would doing so mean another step forward in the advancement of precision medicine, but clinical laboratories and pathology groups also would have new tools to help diagnose disease and guide treatment decisions.
—Andrea Downing Peck
Related Information:
Predicting Risk for Common Deadly Diseases from Millions of Genetic Variants
Multigene Test May Find Risk for Heart Disease and More
A Harvard Scientist Thinks He Has a Gene Test for Heart Attack Risk. He Wants to Give It Away Free



