Telemedicine and Microhospitals Could Make Up for Reducing Numbers of Primary Care Physicians in US Urban and Metro Suburban Areas
Microhospitals already offer most of the critical features of traditional hospitals, and by featuring telemedicine technology at the point of care, they are becoming powerful tools for healthcare providers
Dark Daily reported in January that microhospitals are opening nationwide, including in such innovative states as Texas, Colorado, Nevada, and Arizona. In addition to being open 24/7 and mostly located in high-density areas, these scaled down hospitals feature the most critical aspects of full-size hospitals—medical laboratories, emergency departments, pharmacies, and imaging centers.
However, a report by the Health Resources and Service Administration (HRSA) predicted that by 2020 the US will be short as many as 20,000 primary care physicians! Many specialty practices also are expected to see stiff shortages of physicians in the near future. Without enough physicians, even microhospitals cannot provide adequate care.
Thus, the ever increasing practice of using telemedicine as a way to serve more people, while providing faster, more efficient care tailored to meet the needs of individuals and communities, is welcomed news. If this trend becomes more widespread, it will create new opportunities and challenges for clinical laboratories in hospitals, as well as health systems that own and operate microhospitals.
Filling a Need in Vulnerable Communities
At the end of 2016, there were approximately 50 microhospitals operating in the United States, mostly in the Midwest, Arizona, Colorado, Nevada, and Texas. Sometimes referred to as neighborhood or community hospitals, microhospitals are acute care facilities that are smaller than traditional hospitals but can deliver many of the same medical services. They provide more comprehensive treatments than typical urgent care and outpatient centers and fill a gap between freestanding healthcare centers and major hospitals.
Microhospitals typically have less than a dozen short-stay beds and have the ability to provide inpatient care, emergency care, and imaging and medical laboratory services. And, they are usually affiliated with larger healthcare systems, which allows them to expand into certain areas without incurring the high costs of building a full-scale hospital.
“Right now they seem to be popping up in large urban and suburban metro areas,” Priya Bathija, Vice President, Value Initiative American Hospital Association, told NPR. “We really think they have the potential to help in vulnerable communities that have a lack of access.”
Patient Satisfaction and Declining Physician Populations Drive Demand for Telemedicine
Telemedicine, a combination of telecommunications and information technology, is primarily used to remotely connect healthcare providers to patients during office visits. But it also is being used successfully at the point of care in emergency departments and even surgery.
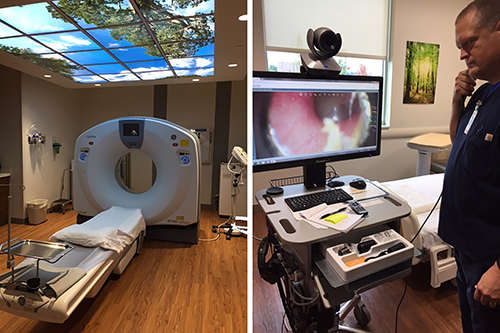
Microhospitals like St. Vincent Neighborhood hospital in Noblesville, Ind., which offer most of the critical functions of traditional hospitals, such as clinical laboratories, ERs, and the CT scanning station above (left), are increasingly including telemedicine technologies (above right) at the point of care to offset reductions in primary care and specialty physicians. (Photo copyright: Jill Sheridan/IPB News.)
Consumers are becoming more accepting of telemedicine (AKA, telehealth) as these services offer savings in both time and money. A recent survey by the Health Industry Distributors Association (HIDA) found that many patients were pleased with telehealth services. More than 50% of the surveyed individuals stated they were very satisfied with a recent telemedicine encounter. In addition, 54% of those individuals described their telehealth experience as better than a traditional, in-person office visit.
Telemedicine and Microhospitals Mutually Beneficial, According to HRSA
Other research suggests microhospitals may generate a mutually beneficial alliance with telemedicine that increases the progress of both entities, especially when considering projected increases in the number of nurse practitioners and physician assistants.
In its report, “Projecting the Supply and Demand for Primary Care Practitioners Through 2020,” Health Resources and Service Administration (HRSA) estimates there will be a shortage of more than 20,000 primary care physicians working in the US by the year 2020. Other specialties expected to experience staff shortfalls include:
- Intensivist;
- Pulmonology;
- Neurology;
- Cardiology; and,
- Psychiatry.
Anticipation of this decline in physician numbers is fueling the demand for telemedicine to help with patient loads, especially in remote areas.
Saving Time and Money with Televisits
A study by Nemours Children’s Health System indicates that telemedicine may reduce medical costs for both patients and healthcare providers while sustaining patient satisfaction.
“At Nemours, we’ve seen how telemedicine can positively impact patients’ lives,” Shayan Vyas, MD, Medical Director of Telehealth at Nemours, noted in a press release. “The overwhelmingly positive response we’ve seen from parents who are early adopters of telemedicine really reinforces the feasibility of online doctor visits and sets the stage for real change in the way healthcare is delivered.”
The Nemours study involved 120 patients under the age of 18. The majority of families surveyed stated they would be interested in future telehealth visits and an impressive 99% said they would recommend telemedicine to other families.
The study discovered that patients and family members saved an average of $50 and about an hour of time, by utilizing telehealth for sports medicine appointments. The health system also experienced some monetary perks with the televisits, as they cost approximately $24 less per patient.
“We know that telemedicine is often looked to for common childhood ailments, like cold and flu, or skin rashes. But we wanted to look at how telemedicine could benefit patients within a particular specialty such as sports medicine,” Alfred Atanda Jr, MD, Pediatric Orthopedic Surgeon at Nemours/Alfred I. DuPont Hospital for Children in Wilmington, DE., told FierceHealthcare. “As the healthcare landscape continues to evolve and the emphasis on value and satisfaction continues to grow, telemedicine may be utilized by providers as a mechanism to keep costs and resource utilization low, and to comply with payer requirements.”
Healthcare consumers and providers are increasing looking to technology to enhance medical care and solve resource shortfalls. Separately, telehealth and microhospitals already help with these needs, Combined, however, they are a powerful solution to our nation’s reducing ranks of primary care physicians and medical specialists.
If this trend of microhospitals using telemedicine should continue and increase, both components will give medical professionals vital tools to provide faster, more economical, and more personalized services, to more patients across wider areas of America.
—JP Schlingman
Related Information:
Why Telehealth is Fueling the Move Towards Microhospitals
Projecting the Supply and Demand for Primary Care Practitioners Through 2020
Are Microhospitals the Answer for Systems Looking for Low-cost Expansions? They Might Be
Microhospitals: Healthcare’s Newest Patient Access Point
Microhospitals Could Prove Financial Boon and Salvation to Healthcare Systems
Microhospitals Provide Health Care Closer to Home
Telemedicine Saves Patients Time and Money, Study Shows
5 Common Questions about Micro-Hospitals, Answered
Survey: More than Half of Patients Prefer Telehealth Visits to In-Person Care
Majority of Parents Plan to Use Telemedicine for Pediatric Care
Microhospitals May Help Deliver Care in Underserved Areas




