Dec 5, 2018 | Laboratory Pathology, Laboratory Testing
Until now, blood doping by athletes to increase performance has been difficult to detect by organizations dedicated to doping-free sports
Research into DNA and RNA keeps resulting in potential new opportunities for anatomic pathologists and clinical laboratories to conduct more precise testing. One recent example comes from Duke University (Duke) where researchers announced they’ve created microRNA-based tests that could be used to monitor blood doping in athletes, a news release reported.
According to the researchers, the finding could reveal athletes who removed their blood, took out the red blood cells, and transfused the cells into their bodies before competition. When conducted by medical laboratory professionals, such autologous blood therapies can enhance oxygen intake and increase performance during sports. However, these “self-transfusions” have been difficult to detect using current methods and that highlights the importance of ensuring these procedures are carried out by authorized healthcare facilities.
The researchers published their findings in the British Journal of Haemotology.
Research Focuses on RNA in Red Blood Cells
The World Anti-Doping Agency (WADA), an international organization aimed at research and education for doping-free sport, funded the Duke University research. WADA currently uses the Athlete Biological Passport to assess, over time, competitors’ body chemistries.
As the Duke researchers explored nucleic acids in red blood cells, they found that the cells actually do have a nucleus, contrary to popular belief. From there, they honed in on RNA.
Short RNA pieces, called microRNA (miRNA), control production of proteins in a cell, according to the researchers.
“While once thought to lack nucleic acids, red blood cells actually contain diverse and abundant RNA species,” the scientists noted in their paper. “In addition, proteomic analyses of red blood cells have identified the presence of Argonaute 2 (AGO2), supporting the regulatory function of miRNAs.”
The methodology Duke researchers followed involved these steps, among others:
- Three units of blood were drawn from volunteers;
- The researchers removed the white blood cells and about 80% of the plasma;
- The remaining red blood cells were pure, just as they would need to be by someone doing autologous transfusion;
- The researchers analyzed cell RNA samples at specific daily intervals: 1, 3, 7, 10, 14, 28, 36, and, 42 days;
- They then compared samples to day 1 and recorded changes in RNA due to storage.
The researchers found:
- Two types of miRNA increased during storage and two declined; and,
- miR-720 had the most dramatic and consistent changes.
They concluded that finding increased miR-720 in athletes’ blood could be used as a biomarker for detecting stored red blood cells, which could indicate blood doping had taken place.

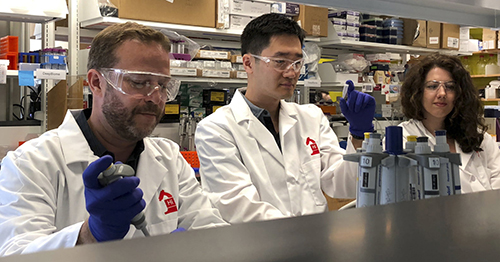
“The difficulty has been that the tests [WADA] have couldn’t tell the difference between a young blood cell and an old one,” Jen-Tsan Ashley Chi, MD, PhD, lead researcher on the study and Duke’s Associate Professor in Molecular Genetics and Microbiology, noted in the news release. “This increase in miR-720 is significant enough and consistent enough that it could be used as a biomarker for detecting stored red blood cells.” Chi is affiliated with Duke’s Center for Genomic and Computational Biology. (Photo copyright: Duke University.)
How does this help clinical laboratories detect blood doping in athletes?
The researchers explained that RNA changes were, indeed, tell-tale signs of old blood cells circulating with normal cells. Those old blood cells could identify an athlete who did a self-transfusion of their blood before a competition.
However, before the test is used in sports more research is needed. Activity by the enzyme angiogenin in stored cells also is worthy of more exploration, as is its role in breaking apart larger RNA, the researchers noted.
“While autologous blood transfusions in athletes is very difficult to identify using conventional tests, it may be detectable based on the presence of red blood cells with levels of miR-720 significantly higher than the normal circulating cells. Further investigations will be necessary to identify the signals during red blood cell storage that stimulate angiogenin activation,” the study paper concluded.
Clinical Laboratories Involved in Sports Testing
In its 2017 Anti-Doping Testing Figures Report, WADA reported 322,050 samples were analyzed, a 7.1% increase from 300,565 samples in 2016. WADA accredits medical laboratories worldwide for conducting such analyses according to the organization’s code. This presents opportunities in sports medicine for medical laboratories to increase revenue through a new line of diagnostic tests.
In fact, the University of California-Los Angeles (UCLA) Olympic Analytical Laboratory is the world’s largest WADA-accredited sports testing facility. Clinical laboratory leaders interested in performing analyses of doping controls for sports—according to WADA’s standards—can contact the organization for its accreditation process.
The Duke study exemplifies how clinical laboratories can extend their services beyond patient care and enter a new realm of leveling playing fields worldwide.
—Donna Marie Pocius
Related Information:
New Finding Could Unmask Blood Doping in Athletes
Angiogenin-mediated tRNA Cleavage as a Novel Feature of Stored Red Blood Cells
Blood and Blood Components
2017 Anti-Doping Testing Figures Report
WADA Accreditation Process
Nov 7, 2018 | Instruments & Equipment, Laboratory Instruments & Laboratory Equipment, Laboratory News, Laboratory Pathology, Laboratory Testing, Management & Operations
CRISPR-Cas9 connection to cancer prompts research to investigate different approaches to gene editing
Dark Daily has covered CRISPR-Cas9 many times in previous e-briefings. Since its discovery, CRISPR, or Clustered Regularly Interspaced Short Palindromic Repeats, has been at the root of astonishing breakthroughs in genetic research. It appears to fulfill precision medicine goals for patients with conditions caused by genetic mutations and has anatomic pathologists, along with the entire scientific world, abuzz with the possibilities such a tool could bring to diagnostic medicine.
All of this research has contributed to a deeper understanding of how cells function. However, as is often the case with new technologies, unforeseen and problematic questions also have arisen.
CRISPR-Cas9 Connection to Cancer
Research conducted at the Wellcome Sanger Institute in the United Kingdom (UK) and published in Nature Biotechnology, examined potential damage caused by CRISPR-Cas9 editing.
“Here we report significant on-target mutagenesis, such as large deletions and more complex genomic rearrangements at the targeted sites in mouse embryonic stem cells, mouse hematopoietic progenitors, and a human differentiated cell line,” wrote the authors in their introduction.
Another study, this one conducted by biomedical researches at Cambridge, Mass., and published in Nature, describes possible toxicity caused by Cas9.
“Our results indicate that Cas9 toxicity creates an obstacle to the high-throughput use of CRISPR-Cas9 for genome engineering and screening in hPSCs [human pluripotent stem cells]. Moreover, as hPSCs can acquire P53 mutations, cell replacement therapies using CRISPR-Cas9-enginereed hPSCs should proceed with caution, and such engineered hPSCs should be monitored for P53 function.”
Essentially what both groups of researchers found is that CRISPR-Cas9 cuts through the double helix of DNA, which the cell responds to as it would any injury. A gene called p53 then directs a cellular “first-aid kit” to the “injury” site that either initiates self-destruction of the cell or repairs the DNA.
Therefore, in some instances, CRISPR-Cas9 is inefficient because the repaired cells continue to function. And, the repair process involves the p53 gene. P53 mutations have been implicated in ovarian, colorectal, lung, pancreatic, stomach, liver, and breast cancers.
Though important, some experts are downplaying the significance of the findings.

Erik Sontheimer, PhD (above), Professor, RNA Therapeutics Institute, at the University of Massachusetts Medical School, told Scientific American that the two studies are important, but not show-stoppers. “This is something that bears paying attention to, but I don’t think it’s a deal-breaker,” he said. (Photo copyright: University of Massachusetts.)
“It’s something we need to pay attention to, especially as CRISPR expands to more diseases. We need to do the work and make sure edited cells returned to patients don’t become cancerous,” Sam Kulkarni, PhD, CEO of CRISPR Therapeutics, told Scientific American.
Both studies are preliminary. The implications, however, is in how genes that have become corrupted are used.
“It is unclear if the findings translate into cells actually used in clinical studies,” Bernhard Schmierer, PhD, co-author of a paper titled, “CRISPR-Cas9 Genome Editing Induces a p53-mediated DNA Damage Response,” told Scientific American.
Nevertheless, the cancer-cat is out of the bag.
Targeting RNA Instead of DNA with CRISPR-Cas13d
A team from the Salk Institute may have found a solution. They are investigating a different enzyme—Cas13d—which, in conjunction with CRISPR would target RNA rather than DNA. “DNA is constant, but what’s always changing are the RNA messages that are copied from the DNA. Being able to modulate those messages by directly controlling the RNA has important implications for influencing a cell’s fate,” Silvana Konermann, PhD, a Howard Hughes Medical Institute (HHMI) Hanna Gray Fellow and member of the research team at Salk, said in a news release.
The Salk team published their findings in the journal Cell. The paper describes how “scientists from the Salk Institute are reporting for the first time the detailed molecular structure of CRISPR-Cas13d, a promising enzyme for emerging RNA-editing technology. They were able to visualize the enzyme thanks to cryo-electron microscopy (cryo-EM), a cutting-edge technology that enables researchers to capture the structure of complex molecules in unprecedented detail.”
The researchers think that CRISPR-Cas13d may be a way to make the process of gene editing more effective and allow for new strategies to emerge. Much like how CRISPR-Cas9 led to research into recording a cell’s history and to tools like SHERLOCK (Specific High-sensitivity Enzymatic Reporter unLOCKing), a new diagnostic tool that works with CRISPR and changed clinical laboratory diagnostics in a foundational way.
Dark Daily reported on this breakthrough last year. (See, “CRISPR-Related Tool Set to Fundamentally Change Clinical Laboratory Diagnostics, Especially in Rural and Remote Locations,” August 4, 2017.)
Each discovery will lead to more branches of inquiry and, hopefully, someday it will be possible to cure conditions like sickle cell anemia, dementia, and cystic fibrosis. Given the high expectations that CRISPR and related technologies can eventually be used to treat patients, pathologists and medical laboratory professionals will want to stay informed about future developments.
—Dava Stewart
Related Information:
Repair of Double-Strand Breaks Induced by CRISPR-Cas9 Leads to Large Deletions and Complex Rearrangements
P53 Inhibits CRISPR-Cas9 Engineering in Human Pluripotent Stem Cells
CRISPR-Edited Cells Linked to Cancer Risk in 2 Studies
CRISPR-Cas9 Genome Editing Induces a p53-Mediated DNA Damage Response
Decoding the Structure of an RNA-Based CRISPR System
Structural Basis for the RNA-Guided Ribonuclease Activity of CRISPR-Cas13d
CRISPR Timeline
What Are Genome Editing and CRISPR-Cas9?
Federal Court Sides with Broad in CRISPR Patent Dispute
Top Biologists Call for Moratorium on Use of CRISPR Gene Editing Tool for Clinical Purposes Because of Concerns about Unresolved Ethical Issues
CRISPR-Related Tool Set to Fundamentally Change Clinical Laboratory Diagnostics, Especially in Rural and Remote Locations
Researchers at Several Top Universities Unveil CRISPR-Based Diagnostics That Show Great Promise for Clinical Laboratories
Aug 15, 2018 | Digital Pathology, Laboratory Management and Operations, Laboratory News, Laboratory Operations, Laboratory Pathology, Laboratory Testing
Using precision genomics, Mayo researchers hope to develop improved medical laboratory tools for screening, diagnosing, and treating patients with inherited genetic disorders such as accelerated aging
Telomeres increasingly are on the radars of physicians and healthcare consumers alike, as researchers gain more knowledge about these critical nucleotides, and doctors continue to indicate their belief that telomeres could make useful diagnostic tools. If so, that would open up a new channel of precision medicine testing for clinical laboratories and anatomic pathology groups.
Telomeres are DNA strands that protect chromosome end points from degrading as people age. Their job is similar to the way plastic tips keep shoelaces from fraying, researchers at the Mayo Clinic explained in a news release. They have been using precision genomics in their assessment of 17 patients with short telomere syndrome (STS) to uncover the genetic causes of the condition.
They published their findings in the July issue of Mayo Clinic Proceedings.
Using Genetic Sequencing to Find Causes of Short Telomeres
People with STS could develop conditions including bone marrow failure, liver disease, and lung disease earlier in life than others, the news release pointed out.
However, according to the researchers’ paper, “Management of STSs is fraught with significant challenges such as delayed diagnoses, lack of routinely available diagnostics modalities, and standardized treatment guidelines.”
Nevertheless, some physicians are already leveraging information about telomeres in patient treatment. And many consumers have been turning to telomere diagnostic testing companies to learn the lengths of their own telomeres. They’ve learned that the longer the telomeres the better, as shorter telomeres are associated with accelerated aging.

“The length of certain telomeres gives a history of all the assaults a person has been subject to over the course of her lifetime,” a Wired article noted, quoting Joseph Raffaele, MD, co-founder of PhysioAge Medical Group, a clinical practice in New York City that specializes in “proactive” medicines. He goes on to call telomeres “the new cholesterol.” (Photo copyright: drraffaele.com.)
More Study into STS is Needed
GenomeWeb summarized the Mayo study’s methodology as follows:
Researchers reported these findings in Mayo Clinic Proceedings:
Study authors concluded that while some genetic mutations are common to short telomeres, they were found in only about 40% of the people in their study. So, more research is needed to discover other causes of short telomeres.
Telomeres and Lung Disease
Other research into telomeres was conducted by St. Paul’s Hospital and the University of British Columbia Department of Medicine, which focused on telomeres and lung disease.
In this study, researchers used polymerase chain reaction (PCR) to measure absolute telomere length from blood samples provided by 576 people with chronic obstructive pulmonary disease (COPD), according to a paper in the journal CHEST, published by the American College of Chest Physicians.
The study found that when compared to people with normal blood telomeres, people with shorter telomere lengths and more rapidly aging blood cells:
- Were 50% more likely to develop new or increasing respiratory symptoms;
- Were nine times more likely to die; and,
- Had worse health status and quality of life.
“It is known that short telomeres are associated with common morbidities of COPD, but it was not known if there is a relationship between blood telomeres and patient-related outcomes in COPD,” Don Sin, MD, a chest physician who led the research at the Centre for Heart Lung Innovation at St. Paul’s Hospital, stated in a news release.
Other Takes on Telomeres
A Harvard Medical blog noted, however, that short telomeres do not necessarily mean disease is imminent, nor that long ones guarantee optimal health.
“There is mounting evidence that a healthy lifestyle buffers your telomeres,” stated Immaculata De Vivo, PhD, a Harvard Medical School Professor and Genetics Researcher at the Dana-Farber/Harvard Cancer Center, in the blog post.
However, another expert questions the value of measuring telomeres for disease risk.
“In short, telomere lengths are too variable within a population, too variable within an individual, and too sensitive to environmental factors to offer any reliable information for common disease risk,” wrote Ricki Lewis, PhD, in PLOS.
Although there are many pitfalls to overcome, some doctors are pushing to use telomere information in patient treatment, and these studies from the Mayo Clinic and other researchers have contributed important data for diagnostic test developers.
In the end, vast and varied content about telomeres exists and clinical laboratory professionals may be called on to help clarify and assess the information. And that’s the long and the short of it.
—Donna Marie Pocius
Related Information:
Precision Genomics Point the Way to Mutations Associated with Accelerated Aging
Telomeres Are the New Cholesterol. Now What?
Clinical Correlates and Treatment Outcomes for Patients with Short Telomeres Syndrome
Mayo Clinic Researchers Use Targeted Sequencing to Diagnose Short Telomere Syndrome
Relationship of Absolute Telomere Length with Quality of Life, Exacerbations, and Mortality in COPD
Blood Telomeres Can Help Predict Risk of Disease Worsening or Death in COPD Patients
Can DNA Markers Called Telomeres Predict Aging?
Telomere Testing: Science or Snake Oil?
White Paper Download | How Next-Generation Sequencing Helps Molecular Laboratories Deliver Personalized Medicine Services to their Client Physicians
Summit: Breakthroughs with Genetic and Precision Medicine: What All Health Network CEOs Need to Know
Aug 6, 2018 | Digital Pathology, Instruments & Equipment, Laboratory Instruments & Laboratory Equipment, Laboratory Management and Operations, Laboratory News, Laboratory Operations, Laboratory Pathology, Laboratory Testing
Researchers in Boston are working to develop DNA as a low-cost, effective way to store data; could lead to new molecular technology industries outside of healthcare
Even as new insights about the role of DNA in various human diseases and health conditions continue to tumble out of research labs, a potential new use for DNA is emerging. A research team in Boston is exploring how to use DNA as a low-cost, reliable way to store and retrieve data.
This has implications for the nation’s clinical laboratories and anatomic pathology groups, because they are gaining experience in sequencing DNA, then storing that data for analysis and use in clinical care settings. If a way to use DNA as a data storage methodology was to become reality, it can be expected that medical laboratories will have the skillsets, experience, and information technology infrastructure already in place to offer a DNA-based data storage service. This would be particularly true for patient data and healthcare data.
Finding a way to reduce the cost of data storage is a primary reason why scientists are looking at ways that DNA could be used as a data storage technology. These scientists and technology developers seek ways to alleviate the world’s over-crowded hard drives, cloud servers, and databases. They hope this can be done by developing technologies that store digital information in artificially-made versions of DNA molecules.
The research so far suggests DNA data storage could be used to store data more effectively than existing data storage solutions. If this proves true, DNA-based data storage technologies could play a key role in industries outside of healthcare.
If so, practical knowledge of DNA handling and storage would be critical to these companies’ success. In turn, this could present unique opportunities for medical laboratory professionals.
DNA Data Storage: Durable but Costly
Besides enormous capacity, DNA-based data storage technology offers durability and long shelf life in a compact footprint, compared to other data storage mediums.
“DNA has an information-storage density several orders of magnitude higher than any other known storage technology,” Victor Zhirnov, PhD, Chief Scientist and Director, Semiconductor Research Corporation, told Wired.
However, projected costs are quite high, due to the cost of writing the information into the DNA. However, Catalog Technologies Inc. of Boston thinks it has a solution.
Rather than producing billions of unique bits of DNA, as Microsoft did while developing its own DNA data storage solution, Catalog’s approach is to “cheaply generate large quantities of just a few different DNA molecules, none longer than 30 base pairs. Then [use] billions of enzymatic reactions to encode information into the recombination patterns of those prefab bits of DNA. Instead of mapping one bit to one base pair, bits are arranged in multidimensional matrices, and sets of molecules represent their locations in each matrix.”
The Boston-based company plans to launch an industrial-scale DNA data storage service using a machine that can daily write a terabyte of data by leveraging 500-trillion DNA molecules, according to Wired. Potential customers include the entertainment industry, federal government, and information technology developers.
Catalog is supported by $9 million from investors. However, it is not the only company working on this. Microsoft and other companies are reportedly working on DNA storage projects as well.
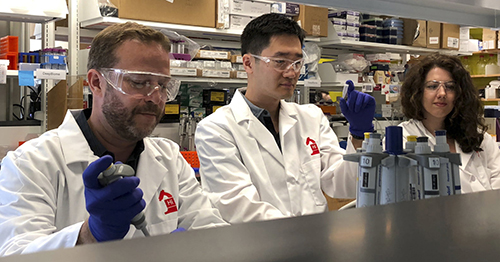
“It’s a new generation of information storage technology that’s got a million times the information density, compared to flash storage. You can shrink down entire data centers into shoeboxes of DNA,” Catalog’s CEO, Hyunjun Park, PhD (above center, between Chief Science Officer Devin Leake on left and Milena Lazova, scientist, on right), told the Boston Globe. (Photo copyright: Catalog.)
Microsoft, University of Washington’s Synthetic DNA Data Storage
Microsoft and researchers at the University of Washington (UW) made progress on their development of a DNA-based storage system for digital data, according to a news release. What makes their work unique, they say, is the large-scale storage of synthetic DNA (200 megabytes) along with the ability to the retrieve data as needed.
“Synthetic DNA is durable and can encode digital data with high density, making it an attractive medium for data storage. However, recovering stored data on a large-scale currently requires all the DNA in a pool to be sequenced, even if only a subset of the information needs to be extracted,” the researchers wrote in their paper published in Nature Biotechnology.
“Here, we encode and store 35 distinct files (over 200 megabytes of data ) in more than 13-million DNA oligonucleotides and show that we can recover each file individually and with no errors, using a random access approach,” the researchers explained.
“Our work reduces the effort, both in sequencing capacity and in processing, to completely recover information stored in DNA,” Sergey Yekhanin, PhD, Microsoft Senior Researcher, told Digital Trends.
Successful research by Catalog, Microsoft, and others may soon lead to the launch of marketable DNA data storage services. And medical laboratory professionals who already know the code—the life code that is—will likely find themselves more marketable as well!
—Donna Marie Pocius
Related Information:
The Rise of DNA Data Storage
The Next Big Thing in Data Storage is Actually Microscopic
Catalog Hauls in $9 Million to Make DNA-Based Data Storage Commercially Viable
UW and Microsoft Researchers Achieve Random Access in Large-Scale DNA Data Storage
Random Access in Large-Scale DNA Data Storage
Microsoft and University of Washington Show DNA Can Store Data in Practical Way
Aug 1, 2018 | Digital Pathology, Instruments & Equipment, Laboratory Instruments & Laboratory Equipment, Laboratory Management and Operations, Laboratory News, Laboratory Operations, Laboratory Pathology, Laboratory Testing, Management & Operations
Identifying patients who will likely develop prolonged concussion symptoms could lead to new clinical laboratory tests and personalized medicine treatments
Researchers are homing in on a new diagnostic assay for concussion that could potentially generate significant numbers of test referrals to the nation’s clinical laboratories. This innovative work is targeting how concussions are diagnosed and treated.
Each year, thousands of children receive sports-related injuries, including concussions. There are ways for anatomic pathologists and hospital medical laboratories to diagnose concussions; however, testing can be invasive and doesn’t always reveal a complete picture of the injury state.
Additionally, about one third of children with concussions develop prolonged symptoms. However, when prescribing treatment plans, physicians have been unable to predict which patients are likely to recover quickly versus those who will have a longer recovery.
Now, researchers at Penn State College of Medicine (Penn State) believe they have discovered five microRNAs in saliva that could be used to identify patients who will likely experience prolonged concussion symptoms even one month after the initial injury.
The study also found that certain materials in saliva can help diagnose the severity of concussions and could hold the key to more effective clinical laboratory tests and personalized medicine treatments.
The Penn State researchers published their study results in JAMA Pediatrics, a publication of the Journal of the American Medical Association (JAMA).
Concussion Leading Sports-related Brain Injury
There are approximately 3.8 million sports and recreation-related traumatic brain injuries in the United States each year and the majority of those cases are concussions, according to The Concussion Place. Most concussions treated in emergency rooms are due to falls, motor-vehicle related injuries, being struck by an object, assaults, or playing sports.
Also known as mild traumatic brain injuries (mTBI), concussions are caused by blows or jolts to the head or body that cause the brain to move with excessive force inside the skull. The sudden impact damages brain cells and causes chemical changes within the brain that alter normal functioning. Though usually not life threatening, the damage can be serious and linger for months.
Symptoms of concussion include: headaches, fatigue, nausea, vomiting, dizziness, balance problems, confusion, memory problems, sleep disturbances, and double or blurry vision. Symptoms usually occur immediately, but could take days or even weeks to appear.
Identifying Severity/Predicting Prolonged Symptoms of Traumatic Brain Injuries
After a concussion occurs, brain cells release small fragments of genetic material known as microRNAs while they attempt to repair themselves. A portion of these microRNAs appear in the injured person’s blood and saliva.
In order to determine whether these microRNAs could be used to determine the severity of a traumatic brain injury and predict whether prolonged symptoms would occur, the prospective cohort study researchers gathered saliva samples from 52 concussion patients between the ages of seven and 21:
- The average age of the subjects was 14;
- Twenty-two of the participants were female;
- They were all athletes; and,
- The majority of the samples were collected one to two weeks after the initial injury.
The researchers examined distinct microRNAs in the samples and identified some that enabled them to predict how long a patient’s concussion symptoms might last. In addition, they found one microRNA in children and young adults that accurately predicted which subjects would experience memory and problem-solving difficulties as part of their symptomatology.
The researchers also evaluated the concussion patients using the Sport Concussion Assessment Tool (SCAT-3), Third Edition. Physicians use this questionnaire to assess the symptoms and severity of concussions. The researchers also asked the parents of the concussed patients for observations about their children’s symptoms.
During follow up visits, which occurred at four- and eight-week increments following the original assessment, the Penn State researchers collected additional saliva samples and re-evaluated the patients using SCAT-3.
New Biomarkers Based on MicroRNAs Instead of Protein
“There’s been a big push recently to find more objective markers that a concussion has occurred, instead of relying simply on patient surveys,” Steven Hicks, MD, PhD, Assistant Professor of Pediatrics, Penn State College of Medicine, Hershey, Pa., one of the study researchers, told Penn State News.
“Previous research has focused on proteins, but this approach is limited because proteins have a hard time crossing the blood-brain barrier. What’s novel about this study is we looked at microRNAs instead of proteins, and we decided to look in saliva rather than blood,” he noted.

According to Steven Hicks, MD, PhD (above), who worked on the Penn State College of Medicine study, microRNAs could be more accurate than the traditional questionnaire when diagnosing and forecasting the effects of concussions. “The microRNAs were able to predict whether symptoms would last beyond four weeks with about 85% accuracy,” he told Penn State News. “In comparison, using the SCAT-3 report of symptoms alone is about 64% accurate. If you just go off the parent’s report of symptoms, it goes down to the mid-50s. In this pilot study, these molecular signatures are outperforming survey tools.” (Photo copyright: MD Magazine.)
The goal of this research was to develop a way to definitively ascertain that a concussion had occurred, predict the length and type of symptoms, and then use that data to improve and personalize care for children and young adults who have had a concussion.
“With that knowledge physicians could make more informed decisions about how long to hold a child out of sports, whether starting more aggressive medication regimens might be warranted, or whether involving a concussion specialist might be appropriate,” Hicks told MD Magazine. “Anytime we can use accurate, objective measures to guide medical care, I think that represents an opportunity to improve concussion treatment.”
Further research and clinical trials will be needed to solidify the effectiveness and accuracy of these new biomarkers. However, a rapid, non-invasive saliva test that can determine the severity of a concussion, and predicted whether prolonged symptoms will likely occur, would be widely used and could be an important assay for clinical laboratories. Particularly those associated with hospital medical laboratories and emergency rooms.
—JP Schlingman
Related Information:
Association of Salivary MicroRNA Changes with Prolonged Concussion Symptoms
Saliva Test May Detect Biomarker for Prolonged Concussion
Molecules in Spit May be Able to Diagnose and Predict Length of Concussions
Prolonged Concussion Symptoms Identifiable by Salivary MicroRNA
Spit Test May Help Reveal Concussion Severity
Saliva Test May Lead to Improved Concussion Care for Youths