Oct 22, 2018 | Digital Pathology, Instruments & Equipment, Laboratory Instruments & Laboratory Equipment, Laboratory Management and Operations, Laboratory News, Laboratory Pathology, Laboratory Testing
UK study shows how LDTs may one day enable physicians to identify patients genetically predisposed to chronic disease and prescribe lifestyle changes before medical treatment becomes necessary
Could genetic predisposition lead to clinical laboratory-developed tests (LDTs) that enable physicians to assess patients’ risk for specific diseases years ahead of onset of symptoms? Could these LDTs inform treatment/lifestyle changes to help reduce the chance of contracting the disease?
A UK study into the genetics of one million people with high blood pressure reveals such tests could one day exist.
Researchers at Queen Mary University of London and Imperial College London uncovered 535 new gene regions affecting hypertension in the largest ever worldwide genetic study of blood pressure, according to a news release.
They also confirmed 274 loci (gene locations) and replicated 92 loci for the first time.
“This is the most major advance in blood pressure genetics to date. We now know that there are over 1,000 genetic signals which influence our blood pressure. This provides us with many new insights into how our bodies regulate blood pressure and has revealed several new opportunities for future drug development,” said Mark Caulfield, MD,
Professor of Clinical Pharmacology at Queen Mary University of London, in the news release. He is also Director of the National Institute for Health Research Barts Biomedical Research Centre.
The researchers believe “this means almost a third of the estimated heritability for blood pressure is now explained,” the news release noted.
Clinical Laboratories May Eventually Get a Genetic Test Panel for Hypertension
Of course, more research is needed. But the study suggests a genetic test panel for hypertension may be in the future for anatomic pathologists and medical laboratories. Physicians might one day be able to determine their patients’ risks for high blood pressure years in advance and advise treatment and lifestyle changes to avert medical problems.
By involving more than one million people, the study also demonstrates how ever-growing pools of data will be used in research to develop new diagnostic assays.
The researchers published their study in Nature Genetics.

The video above summarizes research led by Queen Mary University of London and Imperial College London, which found over 500 new gene regions that influence people’s blood pressure, in the largest global genetic study of blood pressure to date. Click here to view the video. (Photo and caption copyright: Queen Mary University of London.)
Genetics Influence Blood Pressure More Than Previously Thought
In addition to identifying hundreds of new genetic regions influencing blood pressure, the researchers compared people with the highest genetic risk of high blood pressure to those in the low risk group. Based on this comparison, the researchers determined that all genetic variants were associated with:
- “having around a 13 mm Hg higher blood pressure;
- “having 3.34 times the odds for increased risk of hypertension; and,
- “1.52 times the odds for increased risk of poor cardiovascular outcomes.”
“We identify 535 novel blood pressure loci that not only offer new biological insights into blood pressure regulation, but also highlight shared genetic architecture between blood pressure and lifestyle exposures. Our findings identify new biological pathways for blood pressure regulation with potential for improved cardiovascular disease prevention in the future,” the researchers wrote in Nature Genetics.
Other Findings Link Known Genes and Drugs to Hypertension
The UK researchers also revealed the Apolipoprotein E (ApoE) gene’s relation to hypertension. This gene has been associated with both Alzheimer’s and coronary artery diseases, noted Lab Roots. The study also found that Canagliflozin, a drug used in type 2 diabetes treatment, could be repurposed to also address hypertension.
“Identifying genetic signals will increasingly help us to split patients into groups based on their risk of disease,” Paul Elliott, PhD, Professor, Imperial College London Faculty of Medicine, School of Public Health, and co-lead author, stated in the news release. “By identifying those patients who have the greatest underlying risk, we may be able to help them to change lifestyle factors which make them more likely to develop disease, as well as enabling doctors to provide them with targeted treatments earlier.”
Working to Advance Precision Medicine
The study shares new and important information about how genetics may influence blood pressure. By acquiring data from more than one million people, the UK researchers also may be setting a new expectation for research about diagnostic tests that could become part of the test menu at clinical laboratories throughout the world. The work could help physicians and patients understand risk of high blood pressure and how precision medicine and lifestyle changes can possibly work to prevent heart attacks and strokes among people worldwide.
—Donna Marie Pocius
Related Information:
Study of One Million People Leads to World’s Biggest Advance in Blood Pressure Genetics
Researchers Find 535 New Gene Regions That Influence Blood Pressure
Genetic Analysis of Over One Million Identifies 535 New Loci Associated with Blood Pressure Traits
The Facts About High Blood Pressure
High Blood Pressure Breakthrough: Over 500 Genes Uncovered
Study of a Million People Reveals Hypertension Genes
Jul 27, 2018 | Instruments & Equipment, Laboratory Instruments & Laboratory Equipment, Laboratory Management and Operations, Laboratory News, Laboratory Pathology, Management & Operations, News From Dark Daily
Tuft’s proof-of-concept demonstration study shows how changes in saliva can be employed as biomarkers for development of future diagnostic monitoring devices and applications
For years, pathologists and dentists have recognized that the mouth contains many useful biomarkers for a wide range of health conditions and diseases. Now a study by a research team at Tufts University School of Engineering (Tufts) has demonstrated that a tooth-mounted sensor can reliably measure certain target markers.
In this proof-of-concept study, Tufts researchers developed a tooth-mounted sensor that monitors food consumption as it enters the body. This potentially adds behavioral data to the growing list of exploitable biomarkers available to developers of in vitro diagnostics (IVDs) and wearable medical monitoring devices. For that reason, many clinical laboratory managers and anatomic pathologists will want to track further development of this technology, which uses the mouth as the source of the markers to be measured.
A report detailing the device was first published in the scientific journal Advanced Materials in March of this year.
Sensor Reacts to Biomarkers in Saliva
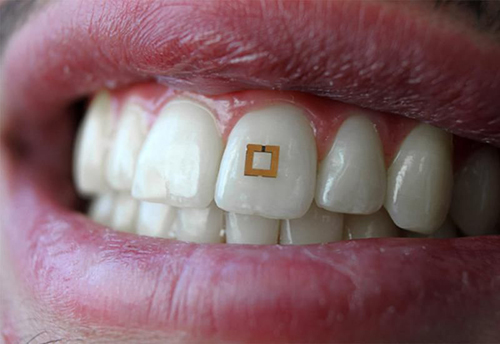
The 2×2-millimeter flexible sensor consists of three layers and adheres to the tooth like a sticker. It has two gold outer rings surrounding an inner layer of bio-responsive material that is highly sensitive to glucose, salt, and alcohol. The presence of any of these substances alters the electrical properties of the sensor and incites it to transmit radio frequency waves that can be received by mobile devices.
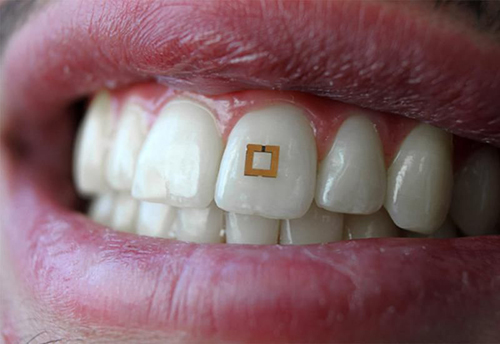
Researchers conducting a proof-of-concept study at Tufts University School of Engineering have developed “a materials‐based strategy to add utility to traditional dielectric sensors by developing a conformal radiofrequency (RF) construct composed of an active layer encapsulated between two reverse‐facing split ring resonators,” their paper published in Advanced Materials notes. The sensor is shown above mounted to a tooth, where it reacts to the presence of certain biomarkers in the saliva, triggering the transmission of an RFID signal. This device has the potential to also measure the same biomarkers used in clinical laboratory tests. (Photo copyright: Smithsonian Magazine/Tufts University School of Engineering.)
There are many possible uses for this tooth-mounted sensor. Individuals with medical conditions such as diabetes, celiac disease, or hypertension, which require them to avoid certain substances in their diet, could benefit from utilizing a device that employs the technology under development at Tufts.
Such a gadget might also help those trying to lose weight. The creators hope to enhance the material, so it has the ability to discern additional nutrients and chemicals.
“If you can evolve the sensor and engineer it to have a database of food consumption, then you could think about nutrition management,” Fiorenzo Omenetto, PhD, Professor, Department of Biomedical Engineering at Tufts and one of the authors of the research told Smithsonian Magazine. “That could be reminding us that we’re indulging too much in sugar or something like that.”
It also could potentially detect physiological or chemical changes taking place in the body by detecting certain bio-markers in the saliva.
“In theory we can modify the bio-responsive layer in these sensors to target other chemicals. We’re really limited only by our creativity,” Omenetto noted in a news release. “We have extended common RFID [radio frequency identification] technology to a sensor package that can dynamically read and transmit information on its environment, whether it is affixed to a tooth, to skin, or any other surface.”
Other Food Intake Devices
There have been previous attempts to develop wearable devices that monitors food intake. However, those gadgets usually required the use of mouth guards and head gear, which are too cumbersome for continuous everyday use. The minute size of the Tufts tooth-mounted device renders it more practical for consumers. And, since it can be mounted anywhere on a tooth—front or back—it can be made undetectable while being worn.
“This study is an interesting proof-of-concept demonstration that small, wireless biosensors can detect changes in saliva due to the presence of compounds such as salt, sugar, and alcohol,” Ben Almquist, PhD, a lecturer in the Department of Bioengineering at Imperial College London, told Smithsonian Magazine.
“For instance, for continuous monitoring of food intake, the sensors will need to be robust enough to withstand abrasion during chewing,” Almquist noted. “In addition, foods are complex mixtures of compounds including salts, sugars and proteins, and the relative amounts of each that enter into saliva will depend on factors such as the nature of the food [i.e., cooked versus fresh], the amount of chewing, and the time in the mouth before swallowing.”
The device currently remains in the prototype stage and more testing will be needed to determine its efficacy and durability. However, the emergence of such wearable devices for medical use suggests valuable opportunities for clinical laboratories.
Because data captured from the tooth-mounted device is transmitted wirelessly, clinical laboratories could potentially store and monitor the data, compare the collected data to other medical laboratory test results for the same patient, then communicate that information to clinicians, other caregivers, and even the patients. This would be a new way for clinical laboratories to provide innovative, value-added services to healthcare professionals and consumers.
—JP Schlingman
Related Information:
This Tiny Tooth Sensor Could Keep Track of the Food You Eat
Scientists Develop Tiny Tooth-mounted Sensors That Can Track What You Eat
A New Tooth-mounted Sensor Will Soon Help You Lose Weight
Functional, RF‐Trilayer Sensors for Tooth‐Mounted, Wireless Monitoring of the Oral Cavity and Food Consumption
May 23, 2018 | Digital Pathology, Laboratory Management and Operations, Laboratory News, Laboratory Operations, Laboratory Pathology, Laboratory Testing
Pathologists around the world will be interested to learn that, for the first time in the UK, prostate cancer has surpassed breast cancer in numbers of deaths annually and nearly 40% of prostate cancer diagnoses occur in stages three and four
Early detection of prostate cancer, and the ability to identify its more aggressive forms, are important goals for every nation’s health system. However, a new study in the United Kingdom (UK) will be of interest to all anatomic pathologists handling prostate biopsies. Researchers determined that late diagnosis of prostate cancer is an issue that should be addressed by healthcare policymakers in the UK.
In 2015, deaths due to prostate cancer surpassed those of breast cancer in the UK. According to data from Cancer Research UK, this trend continued into 2016 with 11,631 deaths from prostate cancer and 11,538 deaths from breast cancer. The trend continued even though breast cancer saw roughly 8,000 more new cases in 2015, according to the same data.
Now, a report from Orchid—a UK male cancer charity—highlights a trend that should interest medical laboratories and histopathology (anatomic pathology in the US) groups that analyze prostate cancer samples. They found that 37% of UK prostate cancer cases involved diagnoses in stages three or four.
Late-Stage Diagnosis of Prostate Cancer: The US and UK Compared
“With prostate cancer due to be the most prevalent cancer in the UK within the next 12 years, we are facing a potential crisis in terms of diagnostics, treatment, and patient care,” stated Rebecca Porta, Chief Executive of Orchid, in a press release. “Urgent action needs to be taken now if we are to be in a position to deliver world class outcomes for prostate cancer patients and their families in the future.”

Orchid Chief Executive Rebecca Porta (far right) and her team are shown above receiving a check from the Industrial Agents Society (AIS) to help fund the charity’s research into male specific cancers, such as prostate cancer. (Photo copyright: AIS.)
The latest data from the Centers for Disease Control and Prevention (CDC) on prostate cancer and mortality rates in the US shows an interesting picture. In 2014, 172,258 men received a prostate cancer diagnosis. However, deaths from prostate cancer were at 28,343.
According to Statista, an international statistics portal, the UK is home to more than 32.3-million males. And, Statista’s data shows the US is home to 159.1-million males. This implies that despite the US having nearly five times the number of males, the number of prostate cancer deaths/year in the UK is significantly higher in relation to population size.
Cancer Research UK notes that despite decreasing by 13% in the last decade, prostate cancer mortality rates are still 21% higher than in the 1970s.
Awareness and Early Detection Key Components in the Fight Against Cancer
A study published in BMC Public Health offers one possible explanation for this disparity.
“When compared to analogous countries in Europe, Canada, and Australia, older adults in the UK have markedly different survival outcomes,” noted lead author of the study Sara Macdonald, PhD, Lecturer in Primary Care at the Institute of Health and Wellbeing at the University of Glasgow, Scotland.
“Poorer outcomes in the UK are at least in part attributable to later stage diagnoses,” she explained. “Older adults should be vigilant about cancer. Yet, this is not reflected in the news media coverage of cancer risk. Taken together, invisibility, inaccuracy, and information overload build a skewed picture that cancer is a disease which affects younger people.”
While treatment options have improved in the past decade, early detection is a key part of successful treatment—especially as prostate cancer has both aggressive and slow variants. Effective timely health screening also is of critical concern.
In the US, however, prolific prostatic-specific antigen (PSA) testing and other screenings for chronic disease—particularly within the elderly population—is under increased scrutiny and criticism, which Dark Daily reported on in April. (See, “Kaiser Health News Labels Routine Clinical Laboratory Testing and Other Screening of Elderly Patients an ‘Epidemic’ in US,” April 11, 2018.)
New Tools to Detect Prostate Cancer
Faster diagnosis and the ability to detect whether a prostate cancer is slow or aggressive could help to shift these numbers around the world.
According to BBC News, the NHS hopes to reduce diagnosis times and make the screening process less invasive by using magnetic resonance imaging (MRI). Hashim Ahmed, PhD, Chairman of Urology, Imperial College London, told BBC News, “Fast access to high-quality prostate MRI allows many men to avoid invasive biopsies as well as allowing precision biopsy in those men requiring it to find high-risk tumors much earlier.”
A team from the University of Dundee is trialing a shear wave elastography imaging (SWEI) process to detect prostate tumors as well. Speaking with The Guardian, team leader and Chair of the School of Medicine at The University of Dundee, Dr. Ghulam Nabi, noted, “We have been able to show a stark difference in results between our technology and existing techniques such as MRI. The technique has picked up cancers which MRI did not reveal. We can now see with much greater accuracy what tissue is cancerous, where it is, and what level of treatment it needs. This is a significant step forward.”
Should these tools prove successful, they might help to reverse current trends in the UK and offer greater insight and options for the histopathology groups there, as well as the medical laboratories, oncologists, and other medical specialists helping to treat cancer.
Until then, raising awareness and streamlining both detection and treatment protocols will remain a critical concern, not just in the UK, but around the world as the human population continues to age.
—Jon Stone
Related Information:
Prostate Cancer: Four in 10 Cases Diagnosed Late, Charity Says
New Report Reveals 4 in 10 Prostate Cancer Cases Are Diagnosed Late and an Impending Crisis in Prostate Cancer Provision
Prostate Cancer Deaths Overtake Those from Breast Cancer
Cutting Prostate Cancer Diagnosis Times
Prostate Cancer on the Rise; Time to Revisit Guidelines?
More High-Risk Prostate Cancer Now in the US than Before
Prostate Cancer Breakthrough as UK Team Develops More Accurate Test
Mass Media and Risk Factors for Cancer: The Under-Representation of Age
Kaiser Health News Labels Routine Clinical Laboratory Testing and Other Screening of Elderly Patients an ‘Epidemic’ in US
Genetic Fingerprint Helps Researchers Identify Aggressive Prostate Cancer from Non-aggressive Types and Determine If Treatment Will Be Effective
Jan 31, 2018 | Instruments & Equipment, Laboratory Instruments & Laboratory Equipment, Laboratory Management and Operations, Laboratory News, Laboratory Operations, Laboratory Pathology, Laboratory Testing
Researchers are finding multiple approaches to metabolomic research and development involving disparate technology platforms and instrumentation
Human metabolome has been discovered to be a wealth of medical laboratory biomarkers for diagnosis, therapy, and patient monitoring. Because it can provide a dynamic phenotype of the human body, there are many potential clinical laboratory applications that could arise from metabolomics, the study of metabolites.
Researchers are discovering numerous ways the expanding field of metabolomics could transform the future of healthcare. However, to fully exploit the potential of human metabolome, developers must choose from various approaches to research.
“The metabolites we’re dealing with have vast differences in chemical properties, which means you need multi-platform approaches and various types of instrumentation,” James MacRae, PhD, Head of Metabolomics at the Francis Crick Institute in London, told Technology Networks. “We can either use an untargeted approach—trying to measure as much as possible, generating a metabolic profile—or else a more targeted approach where we are focusing on specific metabolites or pathways,” he added.
A multi-platform approach means different diagnostic technologies required to assess an individual’s various metabolomes, which, potentially, could result in multi-biomarker assays for medical laboratories.
Measuring All Metabolites in a Cell or Bio System
Metabolomics is the study of small molecules located within cells, biofluids, tissues, and organisms. These molecules are known as metabolites, and their functions within a biological system are cumulatively known as the metabolome.
Metabolomics, the study of metabolome, can render a real-time representation of the complete physiology of an organism by examining differences between biological samples based on their metabolite characteristics.
“Metabolomics is the attempt to measure all of the metabolites in a cell or bio system,” explained MacRae in the Technology Networks article. “You have tens of thousands of genes, of which tens of thousands will be expressed—and you also have the proteins expressed from them, which will then also be modified in different ways. And all of these things impact on a relatively small number of metabolites—in the thousands rather than the tens of thousands. Because of that, it’s a very sensitive output for the health or physiology of your sample.
“With that in mind, metabolomics has great potential for application in most, if not all, diseases—from diabetes, heart disease, cancer, HIV, autoimmune disease, parasitology, and host-pathogen interactions,” he added.

The graphic above is taken from a study published in the Journal of the American College of Cardiology (JACC). It notes, “State-of-the-art metabolomic technologies give us the ability to measure thousands of metabolites in biological fluids or biopsies, providing us with a metabolic fingerprint of individual patients. These metabolic profiles may serve as diagnostic and/or prognostic tools that have the potential to significantly alter the management of [chronic disease].” (Image and caption copyright:Journal of the American College of Cardiology.)
• Genomics: the study of DNA and genetic information within a cell;
• Proteomics: the large-scale study of proteins; and,
• Transcriptomics: the study of RNA and differences in mRNA expressions.
Researchers caution that metabolomics should be used in conjunction with other methods to analyze data for the most accurate results.
“Taking everything together—metabolic profiling, targeted assays, label incorporation and computational models, and also trying to associate all of this with proteomics and
genomics and transcriptomic data—that’s really what encapsulates both the power and also the challenges of metabolomics,” MacRae explained.
Metabolome in Precision Medicine
Metabolomics may also have the ability to help researchers and physicians fine-tune therapies to meet the specific needs of individual patients.
“We know we’re all very different and we don’t respond to drugs in the same way, so we could potentially use metabolomics to help select the best treatment for each individual,” Warwick Dunn, PhD, Senior Lecturer in Metabolomics at the University of Birmingham, Director of Mass Spectrometry, Phenome Center Birmingham, and, Co-Director, Birmingham Metabolomics Training Center, UK, told Technology Networks.
“Our genome is generally static and says what might happen in the future. And the metabolome at the other end is the opposite—very dynamic, saying what just happened or could be about the happen,” Dunn explained. “So, we could apply it to identify prognostic biomarkers, for example, to predict if someone is at greater risk of developing diabetes five to ten years from now. And if you know that, you can change their lifestyle or environment to try and prevent it.”
Metabolomics continues to tap the many diagnostic possibilities posed by the human metabolome. And, the resulting human biomarkers derived from the research could result in a rich new vein of medical laboratory assays.
—JP Schlingman
Related Information:
Metabolomics and Health: On the Cusp of a Revolution
‘Metabolomics’ Distinguishes Pancreatic Cancer from Pancreatitis
Using Metabolomics to Prevent Colon Cancer
Applications of Metabolomics
The Emerging Role of Metabolomics in the Diagnosis and Prognosis of Cardiovascular Disease
Metabolomics Takes Another Step Forward as Methodology for Clinical Laboratory Testing with Development of an Assay for the Diagnosis of Concussion
Jul 12, 2017 | Laboratory Instruments & Laboratory Equipment, Laboratory Management and Operations, Laboratory News, Laboratory Operations, Laboratory Pathology, Management & Operations
High-tech hospitals of the future will ‘bring the healing to the patients’ with virtual consultations and remote diagnostic/monitoring services delivering added value to patient care
Hospitals of the future may look nothing like the hospitals of today and those changes could have major implications for clinical pathologists and medical laboratory scientists.
That’s according to Samuel Smits of Gupta Strategists, a consulting firm in the Netherlands that focuses on the four pillars of the healthcare value chain: suppliers, payers, providers, and government institutions.
In an article in The Economist, Smits predicted that traditional hospitals soon will be no more. “We have reached the peak of bringing patients to the healing centers—our hospitals,” he said. “We are on the brink of bringing the healing to patients.”
The article further notes that the technological revolution on the horizon “means abandoning long-held assumptions about the delivery of care, the role of the patient, and what makes a good doctor.” Virtual consultations and remote monitoring will mean fewer patients will need in-hospital care, while those who do will find a facility that operates “more like a cross between a modern airport and a swish hotel, with mobile check-in, self-service kiosks for blood and urine tests and the like, and updates on patients’ and relatives’ phones,” the Economist article states.
Changing How Care is Delivered
The Economist predicts that “as some sophisticated diagnostics, including blood tests and virtual imaging, become available remotely, more patients will receive hospital-quality care without leaving home.”
Patrick Murray, PhD, Senior Director of Worldwide Scientific Affairs for Becton Dickinson Diagnostics in Franklin, NJ, stated in a Clinical Lab Products (CLP) article that technological advances in laboratory testing and diagnosis will enable pathologists to find increasing numbers of ways to deliver added-value to patient care.
“In my opinion, all diseases and conditions—particularly in the areas of overall wellness, women’s health, chronic diseases, and infectious disease—will benefit from the development of new tests and technologies,” Murray stated in the CLP article. “Additionally, new technologies can help meet the need to ensure traceability and seamless communication of test results not only within the lab, but also with the pharmacy, retail clinics, and physician offices, ultimately aiding in better patient management and providing more accurate insights in public health.”
Patient-and-Digital-First Hospitals
While experts predict patient-and-digital-first philosophies to be the future of hospital design, some healthcare systems already have embraced the trend. At Humber River Hospital in Toronto the future is now. An article in Modern Healthcare describes the patient-centered, high-tech, 656-bed facility, which opened in October 2015, as North America’s “first fully digital hospital.” The hospital leverages technology “wherever possible to improve quality, safety, efficiency, and customer service,” the hospital’s website states.

Humber River Hospital (above) in Toronto has been described as North America’s “first digital hospital.” It offers virtual check-in and registration as well as integrated bedside patient computer terminals that enable patients to order meals, adjust lights, play games, and access internet, television, radio, and their patient portal. (Photo copyright: Humber River Hospital.)
Humber River Hospital’s high-tech features include:
- Robotic blood and specimen testing with results available in minutes and sent electronically to the care team with alerts for immediate attention;
- Computerized patient documentation for immediate bedside charting;
- Bedside computers that enable patients to control lights, use telephone and internet, order food, and review their medical, virtual check-in, and registration information;
- A 4,500-square-foot “Command Center” (opens late 2017) will provide real-time data and predictive analytics to improve clinical, operational, and patient outcomes.
Additionally:
- Three-fourths of the hospital’s supply chain is fully automated; and
- Real-time locating systems (RTLS) track wandering patients and improve security for newborns.
Quality, Safety, Efficiency, Customer Service
Despite all the predicted upheaval to the status quo, John Deverill, Managing Partner at GE Healthcare Partners, expects the modern hospital will survive in some form. “There will always be hospitals where patients with complex needs go for multidisciplinary diagnosis and treatment by teams of specialists,” he stated in the Economist article. He does note, however, that stand-alone facilities for specific surgical interventions, such as joint replacements, may become the norm.
However, former Humber River Hospital President and CEO Rueben Devlin, MD, recommends hospitals not assume every high-tech healthcare innovation is worth pursuing.
“The four things that I think about are quality, safety, efficiency, and customer experience,” he stated in the Modern Healthcare article. “People talk about the Internet of things. I think about the Internet of junk. They’re nice toys but they need to show value to healthcare to make it purposeful.”
Anatomic pathology laboratories have a track record for adopting new technologies. Pathologists were early users of the remote telemedicine models, where telepathology systems enabled a pathologist to remotely control the stage and microscope of the pathologist who originated the telepathology session.
Similarly, the current generation of whole-slide imaging and digital pathology systems are gaining regulatory clearance in both Europe and the United States. If this next wave of technological innovations produces a shift in how clinical care is delivered, an opportunity will be created for clinical pathologists and medical laboratory scientists to adopt technologies that deliver added value to patients, including making inpatient hospital stays less likely.
—Andrea Downing Peck
Related Information:
How Hospitals Could Be Rebuilt Better Than Before
The Hospital of the Future Is Here…But it Needs more Gadgets and Bandwidth
Clinical Lab Trends 2016
NASA-like Command Centers are Coming to Hospitals
Will Growth in Number of Tele-ICU Programs in the Nation’s Hospitals Create an Opportunity for Clinical Pathologists to Deliver Added Value?