North Carolina Providers Slow State Effort to Impose Reference Pricing They Claim Could Remove Hundreds of Doctors and Medical Service Providers from the State’s Healthcare Network
North Carolina turned to reference pricing to reduce employee health costs, but hospitals in the Tarheel State fought back
Efforts by North Carolina’s State Health Plan to adopt reference pricing for its state employees have largely failed, due to united opposition to the reimbursement model by the state’s hospitals, Modern Healthcare reported.
Clinical laboratory leaders are aware that reference pricing is a tool employers and health insurer can use to reduce the wide variation different providers charge for the same clinical service. In 2016 our sister publication, The Dark Report, devoted an entire issue to the subject of reference pricing. (See TDR, “The Newest Threat to Lab Revenues: Reference Pricing in Healthcare,” September 6, 2016.)
The Dark Report wrote about the reference pricing pilot conducted by Safeway, the grocery chain, in collaboration with Anthem, Inc. (NYSE:ANTM), the large health insurance company. The reference pricing program had these elements:
- When Safeway employees and their beneficiaries chose a lab that priced its tests below the 60th percentile, the patient qualified for the health plan’s benefits. But if the patient chose a lab with test prices above the 60th percentile, that patient was responsible for the full cost of the test.
- Safeway employees and their beneficiaries were given a real-time price checking tool that they could access by web browser and smart phone. This app, developed by Castlight Health, Inc., of San Francisco, showed the prices each lab in the Safeway/Anthem network charged for the same lab test, along with the percentile price of that test.
As reported in JAMA Internal Medicine, Safeway introduced reference pricing into its health insurance design for 15,000 employees in 2011. Three years later, the company and its employees were spending 32% less for clinical laboratory tests and saved $2.57 million during the years 2011 to 2013.
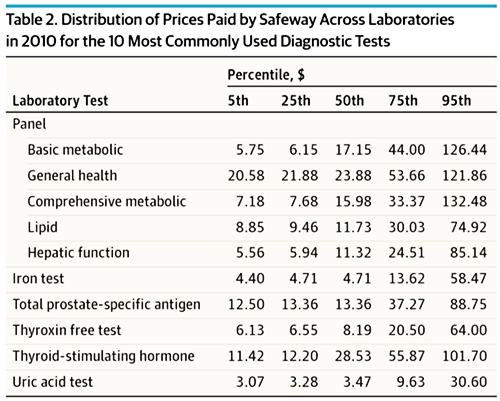
The reference pricing program at Safeway, which focused primarily on clinical laboratory testing, succeeded because of the large variability in how different labs price the same tests. For example, as TDR reported:
- For a basic metabolic panel, which was the most commonly prescribed test, prices among different labs ranged from $5.75 to $126.44; and
- Prices for a lipid panel ranged from $8.85 to $74.92.
Typically, a reference pricing arrangement is done to lower costs, decrease disparities in pricing for similar medical services, and make health plans more attractive to employers. This is why state health plans are looking at implementing reference price reimbursement models as a way to reduce healthcare costs for state employees and other beneficiaries.
North Carolina Providers Respond Negatively to State Reference Pricing Plan
North Carolina’s State Health Plan encountered resistance from the state’s medical community when it attempted to implement a similar reference-price reimbursement model.
The state’s health plan covers more than 727,000 beneficiaries, including teachers, state employees, retired employees, and their dependents. It is overseen by the State Treasurer and administered by BlueCross BlueShield of North Carolina (Blue Cross NC).
In October 2018, North Carolina’s state health plan board of trustees unanimously approved the Clear Pricing Project, a reference-pricing program championed by State Treasurer Dale Folwell. A 2019 Blue Cross NC State Health Plan Network Master Reimbursement Exhibit document states, beginning in 2020, most hospitals would get 160% of the Medicare rate for inpatient services and 230% for outpatient services; rural providers would get more.
Pricing for medical lab and pathology services also was set at 160% of the Medicare rate. The document states, “Except for services identified by Medicare as CLIA Excluded or CLIA Waiver, In-Office Laboratory Service fees will be limited to those services for which you have provided Blue Cross and Blue Shield of North Carolina with evidence of CLIA certification.”
North Carolina’s healthcare providers had no choice but to agree to the pricing to be included in the state’s provider network, but they were not happy about the arrangement.
NCHA Warns Hundreds of Providers Could Be Pushed Out of Network
Hospitals countered with a public relations and lobbying campaign through the North Carolina Healthcare Association (NCHA). Soon after Folwell’s announcement, the NCHA issued a statement claiming that his plan “could force hundreds of providers out of the State Health Plan network or out of business.” The NCHA estimated the potential losses to hospitals and health systems at “upwards of $400 million.”
In the statement, NCHA President Steve Lawler said, “We believe the treasurer is not being transparent about what this proposal will do to state health plan members and their families.”
As an alternative, the NCHA proposed that the state examine value-based approaches such as “case management, outcomes-based payment models, and member education as ways to manage costs.”
The organization established a web page explaining its opposition to the state’s plan and pushed for legislation that would delay its implementation. House Bill 184, which sought to delay implementation of the state’s healthcare reimbursement plan, passed the state House of Representatives in April, before stalling in the Senate in May, North Carolina Health News reported.
Many providers simply refused to sign the necessary contracts, Modern Healthcare reported, even after Folwell agreed to increase the average rate to 196%. In August, he relented and announced that for 2020, the provider network will consist of the North Carolina State Health Plan Network—28,000 providers that had signed on to the Clear Pricing Project—plus the Blue Options PPO Network, which includes providers that had not agreed to the new pricing.
That makes for a total of more than 68,000 providers, states a news release from the treasurer’s office. After the change was announced, providers in the State Health Plan Network were permitted to revert to the Blue Options PPO Network rates.
States may approach implementing reference pricing in different ways, which will likely lead to a distinct disparity in outcomes. Nevertheless, whatever approach is used, medical laboratories and pathology groups will want to understand how reference pricing works and how it may be implemented in their states.
Armed with that understanding, they may want to pursue a proactive strategy of aligning the prices of their lab tests to be at the 50th percentile or lower to avoid being the highest-priced labs in their communities and regions.
—Stephen Beale
Related Information:
NC Aims to Tie Reimbursement to Medicare for State Employees
N.C. Walks Back Reference-Based Pricing Plan for State Workers
State Health Plan Proposed Changes Threaten Healthcare Access for All
North Carolina’s Healthcare Leaders Send Open Letter to NCGA Senators
NCHA Statement on Revised State Health Plan Proposal
NC Healthcare Providers Renew Call for Collaboration on State Health Plan
No Change for State Health Plan Members in 2020
NC State Health Plan Announces Network for 2020
NC State Health Plan Network Increases Payments to Hospitals and Reopens Sign-Up Period
Bill Filed to Stop State Health Plan from Making Health Care Affordable for State Employees
State Health Plan Board of Trustees Unanimously Supports Provider Reimbursement Initiative That Lowers Health Care Costs
State Health Plan Launches New Provider Reimbursement Effort
Plan to Peg State Employee Health Plan Prices to Medicare Rates May Face Legislative Opposition
No More Negotiations: State Health Plan Wants Clearer Process, Lower Prices
On State Health Plan Changes, Folwell Hits Gas While Lawmakers Threaten to Tap Brakes
Treasurer Moves Forward with Health Care Pricing Plan Despite Uncertainty
Lawmakers Derail State Treasurer’s Plan to Change State Health Plan Reimbursement
North Carolina State Health Plan Network Master Reimbursement Exhibit April 2019



